Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
AI in medicine: An analysis of threats, risks, and solutions for the future of healthcare
1
Students’ Scientific Club, Department of Environmental Medicine and Epidemiology, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland
2
Department of Environmental Medicine and Epidemiology, Faculty of Medical Sciences in Zabrze,
Medical University of Silesia, Katowice, Poland
Corresponding author
Helena Brawańska
Studenckie Koło Naukowe, Katedra i Zakład Medycyny i Epidemiologii Środowiskowej, Wydział Nauk Medycznych w Zabrzu ŚUM, ul. Jordana 19, 41-808 Zabrze
Studenckie Koło Naukowe, Katedra i Zakład Medycyny i Epidemiologii Środowiskowej, Wydział Nauk Medycznych w Zabrzu ŚUM, ul. Jordana 19, 41-808 Zabrze
Ann. Acad. Med. Siles. 2025;1(nr specj.):1-11
KEYWORDS
artificial intelligence in medicineAI risksAI ethicsdata securityAI legal regulationsmachine learning
TOPICS
ABSTRACT
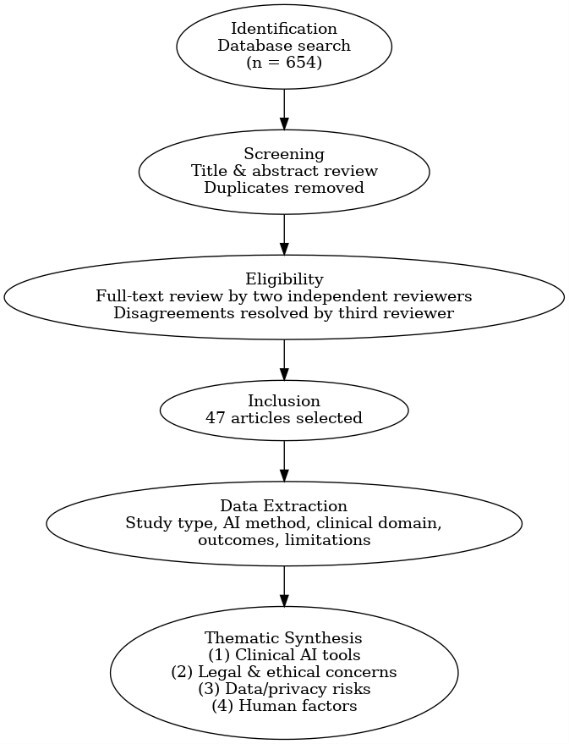
Artificial intelligence (AI) is playing an increasingly significant role in medicine, impacting diagnostics, treatment, and the organization of healthcare systems. This paper analyzes the potential benefits and risks associated with the use of AI in medicine. It focuses on technical, ethical, and regulatory aspects, as well as the impact of AI on patient safety and the effectiveness of clinical decision-making. A comprehensive literature review was conducted in the PubMed, Scopus, and Google Scholar databases, considering publications from 2019 to 2025. A qualitative synthesis of the 52 selected articles identified key challenges and recommendations for further research and implementation of AI in healthcare. The analysis indicates that AI significantly improves diagnostic precision and therapy efficiency, while also posing risks of algorithmic errors, model bias, and breaches of patient privacy. Effective implementation of AI requires legal regulations, clear application guidelines, and multidisciplinary collaboration among experts. Future research should focus on developing mechanisms to increase trust in AI systems and ensure their responsible use in medicine.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding the publication of this paper.
REFERENCES (52)
1.
Lee P., Bubeck S., Petro J. Benefits, limits, and risks of GPT-4 as an AI chatbot for medicine. N. Engl. J. Med. 2023; 388(13): 1233–1239, doi: 10.1056/NEJMsr2214184.
2.
He J., Baxter S.L., Xu J., Xu J., Zhou X., Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat. Med. 2019; 25(1): 30–36, doi: 10.1038/s41591-018-0307-0.
3.
Gomez-Cabello C.A., Borna S., Pressman S., Haider S.A., Haider C.R., Forte A.J. Artificial-Intelligence-based Clinical Decision Support Systems in Primary Care: A scoping review of current clinical implementations. Eur. J. Investig. Health Psychol. Educ. 2024; 14(3): 685–698, doi: 10.3390/ejihpe14030045.
4.
Wang L., Zhang Z., Wang D., Cao W., Zhou X., Zhang P. et al. Human-centered design and evaluation of AI-empowered clinical decision support systems: a systematic review. Front. Comput. Sci. 2023; 5: 1187299, doi: 10.3389/fcomp.2023.1187299.
5.
Davis A., Billick K., Horton K., Jankowski M., Knoll P., Marshall J.E. et al. Artificial intelligence and echocardiography: A primer for cardiac sonographers. J. Am. Soc. Echocardiogr. 2020; 33(9): 1061–1066, doi: 10.1016/j.echo.2020.04.025.
6.
Mintz Y., Brodie R. Introduction to artificial intelligence in medicine. Minim. Invasive Ther. Allied Technol. 2019; 28(2): 73–81, doi: 10.1080/13645706.2019.1575882.
7.
Wang J., Chen Y., Yu S.X., Cheung B., LeCun Y. Compact and optimal deep learning with recurrent parameter generators. In: 2023 IEEE/CVF Winter Conference on Applications of Computer Vision (WACV). IEEE 2023, doi: 10.1109/wacv56688.2023.00389.
8.
Khosravi B., Li F., Dapamede T., Rouzrokh P., Gamble C.U., Trivedi H.M. et al. Synthetically enhanced: unveiling synthetic data’s potential in medical imaging research. EBioMedicine 2024; 104: 105174, doi: 10.1016/j.ebiom.2024.105174.
9.
Tangsrivimol J.A., Darzidehkalani E., Virk H.U.H., Wang Z., Egger J., Wang M. et al. Benefits, limits, and risks of ChatGPT in medicine. Front. Artif. Intell. 2025; 8: 1518049, doi: 10.3389/frai.2025.1518049.
10.
Rajotte J.F., Bergen R., Buckeridge D.L., El Emam K., Ng R., Strome E. Synthetic data as an enabler for machine learning applications in medicine. iScience 2022; 25(11): 105331, doi: 10.1016/j.isci.2022.105331.
11.
Larentzakis A., Lygeros N. Artificial intelligence (AI) in medicine as a strategic valuable tool. Pan Afr. Med. J. 2021; 38: 184, doi: 10.11604/pamj.2021.38.184.28197.
12.
Niewęgłowski K., Wilczek N., Madoń B., Palmi J., Wasyluk M. Zastosowania sztucznej inteligencji (AI) w medycynie. Med. Og. Nauk Zdr. 2021; 27(3): 213–219, doi: 10.26444/monz/142085.
13.
Palaniappan K., Lin E.Y.T., Vogel S. Global regulatory frameworks for the use of artificial intelligence (AI) in the healthcare services sector. Healthcare 2024; 12(5): 562, doi: 10.3390/healthcare12050562.
14.
Wałdoch K. Odpowiedzialność cywilna za szkody wyrządzone w związku z zastosowaniem sztucznej inteligencji w medycynie. [Doctoral thesis]. Uniwersytet Gdański. Gdańsk 2024.
15.
Haug C.J., Drazen J.M. Artificial intelligence and machine learning in clinical medicine, 2023. N. Engl. J. Med. 2023; 388(13): 1201–1208, doi: 10.1056/NEJMra2302038.
16.
Kataoka M., Uematsu T. AI systems for mammography with digital breast tomosynthesis: expectations and challenges. Radiol. Imaging Cancer 2024; 6(4): e240171, doi: 10.1148/rycan.240171.
17.
Regulation (EU) 2024/1689 of the European Parliament and of the Council of 13 June 2024 laying down harmonised rules on artificial intelligence and amending Regulations (EC) No 300/2008, (EU) No 167/2013, (EU) No 168/2013, (EU) 2018/858, (EU) 2018/1139 and (EU) 2019/2144 and Directives 2014/90/EU, (EU) 2016/797 and (EU) 2020/1828 (Artificial Intelligence Act) (Text with EEA relevance). EUR-Lex [online] http://data.europa.eu/eli/reg/... [accessed on May 2025].
18.
Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) (Text with EEA relevance). EUR-Lex [online] http://data.europa.eu/eli/reg/... [accessed on May 2025].
19.
H.R.6216 – National Artificial Intelligence Initiative Act of 2020 (116th Congress [2019–2020]). Congress.gov, 03/12/2020 [online] https://www.congress.gov/bill/... [accessed on May 2025].
20.
Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC (Text with EEA relevance). EUR-Lex [online] http://data.europa.eu/eli/reg/... [accessed on May 2025].
21.
U.S. Food and Drug Administration. Artificial Intelligence/Machine Learning (AI/ML)-Based Software as a Medical Device (SaMD) Action Plan [pdf], January 2021, https://www.fda.gov/media/1450....
22.
Vodanović M., Subašić M., Milošević D., Savić Pavičin I. Artificial intelligence in medicine and dentistry. Acta Stomatol. Croat. 2023; 57(1): 70–84, doi: 10.15644/asc57/1/8.
23.
Bandyopadhyay A., Oks M., Sun H., Prasad B., Rusk S., Jefferson F. et al. Strengths, weaknesses, opportunities, and threats of using AI-enabled technology in sleep medicine: a commentary. J. Clin. Sleep Med. 2024; 20(7): 1183–1191, doi: 10.5664/jcsm.11132.
24.
Cestonaro C., Delicati A., Marcante B., Caenazzo L., Tozzo P. Defining medical liability when artificial intelligence is applied on diagnostic algorithms: a systematic review. Front. Med. 2023; 10: 1305756, doi: 10.3389/fmed.2023.1305756.
25.
Czochra M., Bar D. Śmierć pacjenta wywołana zastosowaniem sztucznej inteligencji w technologiach medycznych – analiza prawnokarna. Stud. Law Res. Paper. 2019; 2(25): 67–81, doi: 10.34697/2451-0807-sp-2019-2-006.
26.
Bączyk-Rozwadowska K. Odpowiedzialność cywilna za szkody wyrzą-dzone w związku z zastosowaniem sztucznej inteligencji w medycynie. PPM 2021; 3(3–4): 5–35, doi: 10.70537/z7xnk378.
27.
Ferry J., Laberge G., Aïvodji U. Learning hybrid interpretable models: Theory, taxonomy, and methods. arXiv. 2023; arXiv: 2303.04437, doi: 10.48550/arXiv.2303.04437.
28.
Wang T., Lin Q. Hybrid predictive models: When an interpretable model collaborates with a black-box model. J. Mach. Learn. Res. 2021; 22(137): 1–38.
29.
Amann J., Blasimme A., Vayena E., Frey D., Madai V.I. et al. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med. Inform. Decis. Mak. 2020; 20(1): 310, doi: 10.1186/s12911-020-01332-6.
30.
Habuza T., Navaz A.N., Hashim F., Alnajjar F., Zaki N., Serhani M.A. et al. AI applications in robotics, diagnostic image analysis and precision medicine: Current limitations, future trends, guidelines on CAD systems for medicine. Inform. Med. Unlocked 2021; 24: 100596, doi: 10.1016/j.imu.2021.100596.
31.
Briganti G., Le Moine O. Artificial intelligence in medicine: today and tomorrow. Front. Med. 2020; 7: 27, doi: 10.3389/fmed.2020.00027.
32.
Kimmerle J., Timm J., Festl-Wietek T., Cress U., Herrmann-Werner A. Medical students’ attitudes toward AI in medicine and their expectations for medical education. J. Med. Educ. Curric. Dev. 2023; 10: 23821205231219346, doi: 10.1177/23821205231219346.
33.
Tomašev N., Glorot X., Rae J.W., Zielinski M., Askham H., Saraiva A. et al. Developing deep learning continuous risk models for early adverse event prediction in electronic health records: an AKI case study. Protocol Exchange 2019, doi: 10.21203/rs.2.10083/v1.
34.
Parikh R.B., Teeple S., Navathe A.S. Addressing bias in artificial intelligence in health care. JAMA 2019; 322(24): 2377–2378, doi: 10.1001/jama.2019.18058.
35.
Homolak J. Opportunities and risks of ChatGPT in medicine, science, and academic publishing: a modern Promethean dilemma. Croat. Med. J. 2023; 64(1): 1–3, doi: 10.3325/cmj.2023.64.1.
36.
De Freitas J., Cohen I.G. The health risks of generative AI-based wellness apps. Nat. Med. 2024; 30(5): 1269–1275, doi: 10.1038/s41591-024-02943-6.
37.
Milne-Ives M., Selby E., Inkster B., Lam C., Meinert E. Artificial intelligence and machine learning in mobile apps for mental health: A scoping review. PLOS Digit. Health 2022; 1(8): e0000079, doi: 10.1371/journal.pdig.0000079.
38.
Ma X., Niu Y., Gu L., Wang Y., Zhao Y., Bailey J. et al. Understanding adversarial attacks on deep learning based medical image analysis systems. Pattern Recognit. 2021; 110: 107332, doi: 10.1016/j.patcog.2020.107332.
39.
Kiener M. Artificial intelligence in medicine and the disclosure of risks. AI Soc. 2020; 36(3): 705–713, doi: 10.1007/s00146-020-01085-w.
40.
Finlayson S.G., Bowers J.D., Ito J., Zittrain J.L., Beam A.L., Kohane I.S. Adversarial attacks on medical machine learning. Science 2019; 363(6433): 1287–1289, doi: 10.1126/science.aaw4399.
41.
Hu H., Salcic Z., Sun L., Dobbie G., Yu P.S., Zhang X. Membership inference attacks on machine learning: A survey. ACM Comput. Surv. 2022; 54(11s): 1–37, doi: 10.1145/3523273.
42.
Newaz A.I., Haque N.I., Sikder A.K., Rahman M.A., Uluagac A.S. Adversarial attacks to machine learning-based smart healthcare systems. GLOBECOM 2020 – 2020 IEEE Global Communications Conference, p. 1–6, doi: 10.1109/GLOBECOM42002.2020.9322472.
43.
Kanter G.P., Packel E.A. Health care privacy risks of AI chatbots. JAMA 2023; 330(4): 311–312, doi: 10.1001/jama.2023.9618.
44.
Rajpurkar P., Chen E., Banerjee O., Topol E.J. AI in health and medicine. Nat. Med. 2022; 28(1): 31–38, doi: 10.1038/s41591-021-01614-0.
45.
Lichosik D. Opieka i leczenie onkologiczne pacjenta w dobie sztucznej inteligencji (AI). [Film / Speech]. Baza Wiedzy Akademii Tarnowskiej, 2024 [online] https://rpt.atar.edu.pl/info/m... 2023.
46.
Barański J. Intelligent revolution in medicine – the application of artificial intelligence (ai) in medicine: overview, benefits, and challenges. Przegl. Epidemiol. 2024; 78(3): 287–302, doi: 10.32394/pe/194484.
47.
Ahmad Z., Rahim S., Zubair M., Abdul-Ghafar J. Artificial intelligence (AI) in medicine, current applications and future role with special emphasis on its potential and promise in pathology: present and future impact, obstacles including costs and acceptance among pathologists, practical and philosophical considerations. A comprehensive review. Diagn. Pathol. 2021; 16(1): 24, doi: 10.1186/s13000-021-01085-4.
48.
Donia J., Shaw J.A. Co-design and ethical artificial intelligence for health: An agenda for critical research and practice. Big Data Soc. 2021; 8(2): 20539517211065248, doi: 10.1177/20539517211065248.
49.
Benz C., Scott-Jeffs W., McKercher K.A., Welsh M., Norman R., Hendrie D. et al. Community-based participatory-research through co-design: supporting collaboration from all sides of disability. Res. Involv. Engagem. 2024; 10(1): 47, doi: 10.1186/s40900-024-00573-3.
50.
Weidener L., Fischer M. Teaching AI ethics in medical education: A scoping review of current literature and practices. Perspect. Med. Educ. 2023; 12(1): 399–410, doi: 10.5334/pme.954.
51.
Alam F., Lim M.A., Zulkipli I.N. Integrating AI in medical education: embracing ethical usage and critical understanding. Front. Med. 2023; 10: 1279707, doi: 10.3389/fmed.2023.1279707.
52.
Biała Księga AI w praktyce klinicznej: stosowanie sztucznej inteligencji przy udzielaniu świadczeń zdrowotnych [pdf]. [Wersja 1.0]. Koalicja AI w Zdrowiu / Grupa Robocza ds. Sztucznej Inteligencji / Polska Federacja Szpitali. wZdrowiu. Warszawa, czerwiec 2022, https://aiwzdrowiu.pl/wp-conte... [accessed on May 2025].
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.