Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Health-promoting strategies and anxiety about long COVID in medical professionals: A cross-sectional survey during the pandemic
1
Department of Medical Biophysics, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
Corresponding author
Barbara Pietrzyk
Katedra i Zakład Biofizyki Lekarskiej, Wydział Nauk Medycznych ŚUM, ul. Medyków 18, 40-752 Katowice
Katedra i Zakład Biofizyki Lekarskiej, Wydział Nauk Medycznych ŚUM, ul. Medyków 18, 40-752 Katowice
Ann. Acad. Med. Siles. 2026;80:1-6
KEYWORDS
TOPICS
ABSTRACT
Introduction:
The coronavirus disease 2019 (COVID-19) pandemic has caused global lifestyle changes. Social isolation measures and rising SARS-CoV-2 complications have significantly affected healthcare workers who face increased occupational demands and growing concerns about infection risks and long-term consequences. This study examined the association between medical profession type and both COVID-19 health behaviors and long-term complication concerns.
Material and methods:
A retrospective study was conducted on a group of 133 healthcare workers and medical students between October 2023 and February 2024. A questionnaire designed by the author was used, which collected demographic and anthropometric data, as well as information on health-promoting behaviors related to the COVID-19 pandemic. Descriptive statistics were used, with significance set at p < 0.05. Comparisons between variables were performed using the Fisher exact test.
Results:
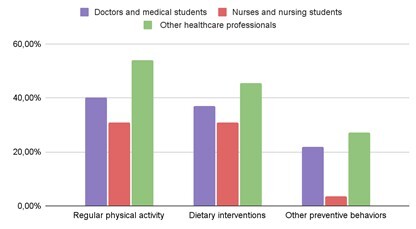
During the COVID-19 pandemic 40.6% of healthcare workers engaged in physical activity, 33.8% modified diets, and 18.8% adopted other preventive behaviors, with no significant profession-dependent differences (p > 0.05). Nearly half (48.9%) expressed long-term complication concerns, most frequently among “other healthcare professionals” (77.3%), showing significant group variation (p = 0.01). Doctors/medical students disproportionately reported ≥ 4 specific concerns (p < 0.05). The study reveals profession-linked disparities in risk perception but not preventive behaviors.
Conclusions:
The study found no profession-dependent differences in COVID-19 preventive behaviors (p > 0.05), but significant variation in long-term complication concerns (p < 0.05). While health measures were uniform across roles, risk perception differed by type of medical profession.
The coronavirus disease 2019 (COVID-19) pandemic has caused global lifestyle changes. Social isolation measures and rising SARS-CoV-2 complications have significantly affected healthcare workers who face increased occupational demands and growing concerns about infection risks and long-term consequences. This study examined the association between medical profession type and both COVID-19 health behaviors and long-term complication concerns.
Material and methods:
A retrospective study was conducted on a group of 133 healthcare workers and medical students between October 2023 and February 2024. A questionnaire designed by the author was used, which collected demographic and anthropometric data, as well as information on health-promoting behaviors related to the COVID-19 pandemic. Descriptive statistics were used, with significance set at p < 0.05. Comparisons between variables were performed using the Fisher exact test.
Results:
During the COVID-19 pandemic 40.6% of healthcare workers engaged in physical activity, 33.8% modified diets, and 18.8% adopted other preventive behaviors, with no significant profession-dependent differences (p > 0.05). Nearly half (48.9%) expressed long-term complication concerns, most frequently among “other healthcare professionals” (77.3%), showing significant group variation (p = 0.01). Doctors/medical students disproportionately reported ≥ 4 specific concerns (p < 0.05). The study reveals profession-linked disparities in risk perception but not preventive behaviors.
Conclusions:
The study found no profession-dependent differences in COVID-19 preventive behaviors (p > 0.05), but significant variation in long-term complication concerns (p < 0.05). While health measures were uniform across roles, risk perception differed by type of medical profession.
REFERENCES (20)
1.
Kraut RE, Li H, Zhu H. Mental health during the COVID-19 pandemic: Impacts of disease, social isolation, and financial stressors. PLoS One. 2022;17(11):e0277562. doi: 10.1371/journal.pone.0277562.
2.
Hadar-Shoval D, Alon-Tirosh M, Asraf K, Tannous-Haddad L, Tzischinsky O. Lifestyle Changes, Emotional Eating, Gender, and Stress during COVID-19 Lockdown. Nutrients. 2022;14(18):3868. doi: 10.3390/nu14183868.
3.
Alon-Tirosh M, Hadar-Shoval D, Asraf K, Tannous-Haddad L, Tzischinsky O. The Association between Lifestyle Changes and Psychological Distress during COVID-19 Lockdown: The Moderating Role of COVID-Related Stressors. Int J Environ Res Public Health. 2021;18(18):9695. doi: 10.3390/ijerph18189695.
4.
Khanji MY, Collett G, Godec T, Maniero C, Ng SM, Siddiqui I, et al. Improved lifestyle is associated with improved depression, anxiety and well-being over time in UK healthcare professionals during the COVID-19 pandemic: insights from the CoPE-HCP cohort study. Gen Psychiatr. 2023;36(1):e100908. doi: 10.1136/gpsych-2022-100908.
5.
Siddiqui I, Gupta J, Collett G, McIntosh I, Komodromos C, Godec T, et al. Perceived workplace support and mental health, well-being and burnout among health care professionals during the COVID-19 pandemic: a cohort analysis. CMAJ Open. 2023;11(1):E191–E200. doi: 10.9778/cmajo.20220191.
6.
Shenkman R, Diewald L, Murray MB, Oliver TL. Unveiling Lived Experiences: Exploring the Health and Lifestyle Effects of COVID-19 on Healthcare Workers. Nutrients. 2023;15(23):4857. doi: 10.3390/nu15234857.
7.
Hannemann J, Abdalrahman A, Erim Y, Morawa E, Jerg-Bretzke L, Beschoner P, et al. The impact of the COVID-19 pandemic on the mental health of medical staff considering the interplay of pandemic burden and psychosocial resources-A rapid systematic review. PLoS One. 2022;17(2):e0264290. doi: 10.1371/journal.pone.0264290.
8.
Fouad MM, Zawilla NH, Maged LA. Work performance among healthcare workers with post COVID-19 syndrome and its relation to antibody response. Infection. 2023;51(4):839–849. doi: 10.1007/s15010-022-01942-4.
9.
Strahm C, Seneghini M, Güsewell S, Egger T, Leal-Neto O, Brucher A, et al. Symptoms Compatible With Long Coronavirus Disease (COVID) in Healthcare Workers With and Without Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection-Results of a Prospective Multicenter Cohort. Clin Infect Dis. 2022;75(1):e1011–e1019. doi: 10.1093/cid/ciac054.
10.
GBD 2021 Demographics Collaborators. Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950–2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):1989–2056. doi: 10.1016/S0140-6736(24)00476-8.
11.
Andrade C. The P Value and Statistical Significance: Misunderstandings, Explanations, Challenges, and Alternatives. Indian J Psychol Med. 2019;41(3):210–215. doi: 10.4103/IJPSYM.IJPSYM_193_19.
12.
Jung SH. Stratified Fisher’s exact test and its sample size calculation. Biom J. 2014;56(1):129–140. doi: 10.1002/bimj.201300048.
13.
Stefanatou P, Xenaki LA, Karagiorgas I, Ntigrintaki AA, Giannouli E, Malogiannis IA, et al. Fear of COVID-19 Impact on Professional Quality of Life among Mental Health Workers. Int J Environ Res Public Health. 2022;19(16):9949. doi: 10.3390/ijerph19169949.
14.
Mulhem E, Zeman LL, Childers K, Roy S, Homayouni R. Association of health behaviors with healthcare workers’ physical and psychological well-being: Learning from the COVID-19 pandemic. PLoS One. 2025;20(10):e0334752. doi: 10.1371/journal.pone.0334752.
15.
Greenberg N, Weston D, Hall C, Caulfield T, Williamson V, Fong K. Mental health of staff working in intensive care during Covid-19. Occup Med (Lond). 2021;71(2):62–67. doi: 10.1093/occmed/kqaa220.
16.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026.
17.
Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212.
18.
Riedel B, Horen SR, Reynolds A, Hamidian Jahromi A. Mental Health Disorders in Nurses During the COVID-19 Pandemic: Implications and Coping Strategies. Front Public Health. 2021;9:707358. doi: 10.3389/fpubh.2021.707358.
19.
Kızılkaya S, Çağatay A. Behind COVID-19 pandemic backstage: anxiety and healthcare workers. Cir Cir. 2023;91(2):247–252. doi: 10.24875/CIRU.22000418.
20.
Gozpinar N, Cakiroglu S, Zorlu A, Yıldırım Budak B, Gormez V. Videoconference anxiety: Conceptualization, scale development, and preliminary validation. Bull Menninger Clin. 2022;86(3):223–248. doi: 10.1521/bumc.2022.86.3.223.
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.