Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
The burden of atherosclerotic cardiovascular disease in an aging population: A comprehensive review of risk factors, risk assessment, and prevention
1
3rd Department of Cardiology, Silesian Centre for Heart Diseases in Zabrze, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland
2
Department of Cardiovascular Disease Prevention, Faculty of Public Health in Bytom, Medical University of Silesia, Katowice, Poland
Corresponding author
Witold Żurański
III Katedra i Klinika Kardiologii, Śląskie Centrum Chorób Serca, ul. Marii Curie-Skłodowskiej 9, 41-800 Zabrze
III Katedra i Klinika Kardiologii, Śląskie Centrum Chorób Serca, ul. Marii Curie-Skłodowskiej 9, 41-800 Zabrze
Ann. Acad. Med. Siles. 2025;79:404-417
KEYWORDS
TOPICS
ABSTRACT
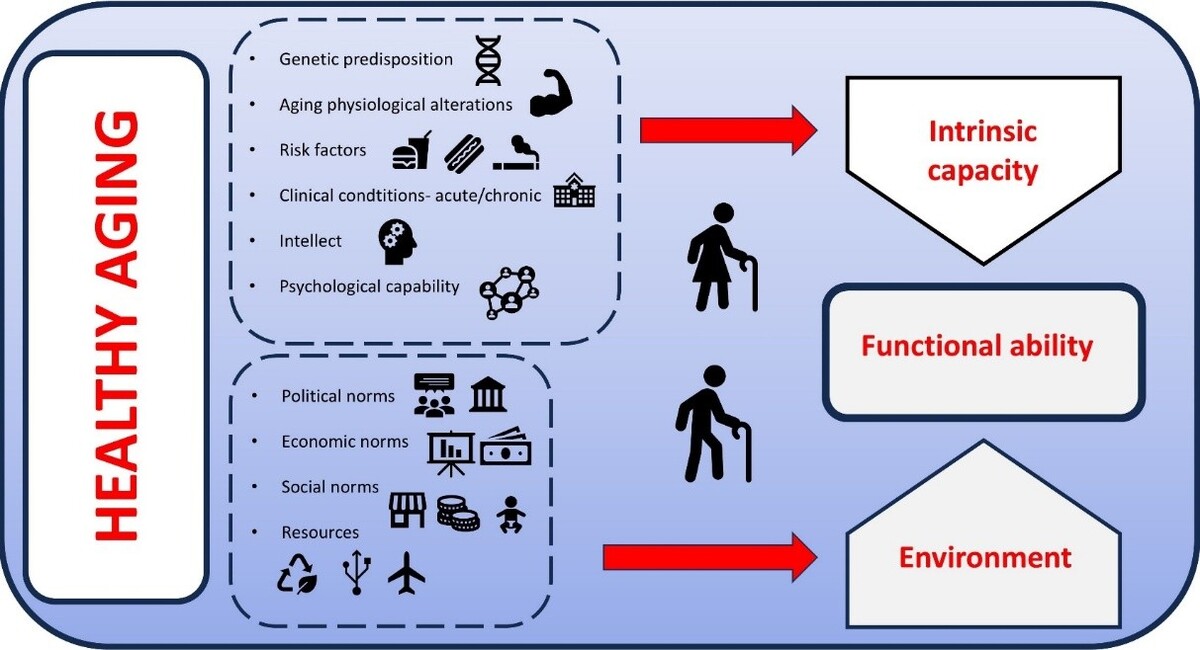
Aging is a key risk factor for atherosclerotic cardiovascular diseases (ASCVDs), leading to high morbidity and mortality among older adults. As the population ages and medical advances prolong survival, more individuals live with ASCVD, necessitating personalized management that addresses complex medical, social, and functional challenges. Besides traditional risk factors, geriatric syndromes and non-cardiovascular comorbidities – commonly referred to as competing risks – significantly impact outcomes. Although assessment tools exist, their clinical use is limited by complexity and patient diversity. Early prevention of geriatric conditions such as frailty, sarcopenia, malnutrition, and multimorbidity is essential to reduce adverse events and cardiovascular risk.
REFERENCES (124)
1.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–3337. doi: 10.1093/eurheartj/ehab484.
2.
Mazzolai L, Teixido-Tura G, Lanzi S, Boc V, Bossone E, Brodmann M, et al. 2024 ESC Guidelines for the management of peripheral arterial and aortic diseases. Eur Heart J. 2024;45(36):3538–3700. doi: 10.1093/eurheartj/ehae179.
3.
Kim KI. Risk Stratification of Cardiovascular Disease according to Age Groups in New Prevention Guidelines: A Review. J Lipid Atheroscler. 2023;12(2):96–105. doi: 10.12997/jla.2023.12.2.96.
4.
Pitkala KH, Strandberg TE. Clinical trials in older people. Age Ageing. 2022;51(5):afab282. doi: 10.1093/ageing/afab282.
5.
Lopes LC, Benko R, Oliveira MG, Paniz VMV, Godman B, Motter FR. Editorial: Evidence for Assessing Drug Safety and Drug Use in Older People. Front Pharmacol. 2022;13:941813. doi: 10.3389/fphar.2022.941813.
6.
Damluji AA, Forman DE, Wang TY, Chikwe J, Kunadian V, Rich MW, et al. Management of Acute Coronary Syndrome in the Older Adult Population: A Scientific Statement From the American Heart Association. Circulation. 2023;147(3):e32–e62. doi: 10.1161/CIR.0000000000001112.
7.
Ageing and Health. World Health Organization [online] https://www.who.int/news-room/... [accessed on 1 October 2022].
8.
Lettino M, Mascherbauer J, Nordaby M, Ziegler A, Collet JP, Derumeaux G, et al. Cardiovascular disease in the elderly: Proceedings of the European Society of Cardiology—Cardiovascular Round Table. Eur J Prev Cardiol. 2022;29(10):1412–1424. doi: 10.1093/eurjpc/zwac033.
9.
Hazra NC, Rudisill C, Gulliford MC. Determinants of health care costs in the senior elderly: age, comorbidity, impairment, or proximity to death? Eur J Health Econ. 2018;19(6):831–842. doi: 10.1007/s10198-017-0926-2.
10.
Martin P, Kelly N, Kahana B, Kahana E, Willcox BJ, Willcox DC, et al. Defining successful aging: a tangible or elusive concept? Gerontologist. 2015;55(1):14–25. doi: 10.1093/geront/gnu044.
11.
Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020;139:6–11. doi: 10.1016/j.maturitas.2020.05.018.
12.
Menassa M, Stronks K, Khatmi F, Roa Díaz ZM, Espinola OP, Gamba M, et al. Concepts and definitions of healthy ageing: a systematic review and synthesis of theoretical models. EClinicalMedicine. 2023;56:101821. doi: 10.1016/j.eclinm.2022.101821.
13.
Mensah GA, Roth GA, Fuster V. The Global Burden of Cardiovascular Diseases and Risk Factors: 2020 and Beyond. J Am Coll Cardiol. 2019;74(20):2529–2532. doi: 10.1016/j.jacc.2019.10.009.
14.
Lucchi T. Dyslipidemia and prevention of atherosclerotic cardiovascular disease in the elderly. Minerva Med. 2021;112(6):804–816. doi: 10.23736/S0026-4806.21.07347-X.
15.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9.
16.
Qu C, Liao S, Zhang J, Cao H, Zhang H, Zhang N, et al. Burden of cardiovascular disease among elderly: based on the Global Burden of Disease Study 2019. Eur Heart J Qual Care Clin Outcomes. 2024;10(2):143–153. doi: 10.1093/ehjqcco/qcad033.
17.
Dong C, Bu X, Liu J, Wei L, Ma A, Wang T. Cardiovascular disease burden attributable to dietary risk factors from 1990 to 2019: A systematic analysis of the Global Burden of Disease study. Nutr Metab Cardiovasc Dis. 2022;32(4):897–907. doi: 10.1016/j.numecd.2021.11.012.
18.
Rosengren A, Smyth A, Rangarajan S, Ramasundarahettige C, Bangdiwala SI, AlHabib KF, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. 2019;7(6):e748–e760. doi: 10.1016/S2214-109X(19)30045-2.
19.
Li Z, Yang Y, Wang X, Yang N, He L, Wang J, et al. Comparative analysis of atherosclerotic cardiovascular disease burden between ages 20–54 and over 55 years: insights from the Global Burden of Disease Study 2019. BMC Med. 2024;22(1):303. doi: 10.1186/s12916-024-03527-4.
20.
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al.; ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–477. doi: 10.1093/eurheartj/ehz425.
21.
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al.; ESC Scientific Document Group. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44(38):3720–3826. doi: 10.1093/eurheartj/ehad191.
22.
Vrints C, Andreotti F, Koskinas KC, Rossello X, Adamo M, Ainslie J, et al.; ESC Scientific Document Group. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur Heart J. 2024;45(36):3415–3537. doi: 10.1093/eurheartj/ehae177.
23.
Wang W, Hu M, Liu H, Zhang X, Li H, Zhou F, et al. Global Burden of Disease Study 2019 suggests that metabolic risk factors are the leading drivers of the burden of ischemic heart disease. Cell Metab. 2021;33(10):1943–1956.e2. doi: 10.1016/j.cmet.2021.08.005.
24.
Safiri S, Karamzad N, Singh K, Carson-Chahhoud K, Adams C, Nejadghaderi SA, et al. Burden of ischemic heart disease and its attributable risk factors in 204 countries and territories, 1990–2019. Eur J Prev Cardiol. 2022;29(2):420–431. doi: 10.1093/eurjpc/zwab213.
25.
Donkor ES. Stroke in the 21st Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res Treat. 2018;2018:3238165. doi: 10.1155/2018/3238165.
26.
GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820. doi: 10.1016/S1474-4422(21)00252-0.
27.
Li XY, Kong XM, Yang CH, Cheng ZF, Lv JJ, Guo H, et al. Global, regional, and national burden of ischemic stroke, 1990–2021: an analysis of data from the global burden of disease study 2021. EClinicalMedicine. 2024;75:102758. doi: 10.1016/j.eclinm.2024.102758.
28.
Zhu W, He X, Huang D, Jiang Y, Hong W, Ke S, et al. Global and Regional Burden of Ischemic Stroke Disease from 1990 to 2021: An Age-Period-Cohort Analysis. Transl Stroke Res. 2025;16(5):1474–1485. doi: 10.1007/s12975-024-01319-9.
29.
He Q, Wang W, Zhang Y, Xiong Y, Tao C, Ma L, et al. Global, Regional, and National Burden of Stroke, 1990–2021: A Systematic Analysis for Global Burden of Disease 2021. Stroke. 2024;55(12):2815–2824. doi: 10.1161/STROKEAHA.124.048033.
30.
Creager MA. A Bon VOYAGER for Peripheral Artery Disease. N Engl J Med. 2020;382(21):2047–2048. doi: 10.1056/NEJMe2007274.
31.
GBD 2019 Peripheral Artery Disease Collaborators. Global burden of peripheral artery disease and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Glob Health. 2023;11(10):e1553–e1565. doi: 10.1016/S2214-109X(23)00355-8.
32.
Eid MA, Mehta K, Barnes JA, Wanken Z, Columbo JA, Stone DH, et al. The global burden of peripheral artery disease. J Vasc Surg. 2023;77(4):1119–1126.e1. doi: 10.1016/j.jvs.2022.12.015.
33.
Zhao D, Guallar E, Ouyang P, Subramanya V, Vaidya D, Ndumele CE, et al. Endogenous Sex Hormones and Incident Cardiovascular Disease in Post-Menopausal Women. J Am Coll Cardiol. 2018;71(22):2555–2566. doi: 10.1016/j.jacc.2018.01.083.
34.
Vogel B, Acevedo M, Appelman Y, Bairey Merz CN, Chieffo A, Figtree GA, et al. The Lancet women and cardiovascular disease Commission: reducing the global burden by 2030. Lancet. 2021;397(10292):2385–2438. doi: 10.1016/S0140-6736(21)00684-X.
35.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al.; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010.
36.
Ma S, Xie X, Yuan R, Xin Q, Miao Y, Leng SX, et al. Vascular Aging and Atherosclerosis: A Perspective on Aging. Aging Dis. 2024;16(1):33–48. doi: 10.14336/AD.2024.0201-1.
37.
Cho MJ, Lee MR, Park JG. Aortic aneurysms: current pathogenesis and therapeutic targets. Exp Mol Med. 2023;55(12):2519–2530. doi: 10.1038/s12276-023-01130-w.
38.
Wang Z, You Y, Yin Z, Bao Q, Lei S, Yu J, et al. Burden of Aortic Aneurysm and Its Attributable Risk Factors from 1990 to 2019: An Analysis of the Global Burden of Disease Study 2019. Front Cardiovasc Med. 2022;9:901225. doi: 10.3389/fcvm.2022.901225.
39.
Krafcik BM, Stone DH, Cai M, Jarmel IA, Eid M, Goodney PP, et al. Changes in global mortality from aortic aneurysm. J Vasc Surg. 2024;80(1):81–88.e1. doi: 10.1016/j.jvs.2024.02.025.
40.
Mistriotis P, Andreadis ST. Vascular aging: Molecular mechanisms and potential treatments for vascular rejuvenation. Ageing Res Rev. 2017;37:94–116. doi: 10.1016/j.arr.2017.05.006.
41.
Tyrrell DJ, Goldstein DR. Ageing and atherosclerosis: vascular intrinsic and extrinsic factors and potential role of IL-6. Nat Rev Cardiol. 2021;18(1):58–68. doi: 10.1038/s41569-020-0431-7.
42.
Li X, Li C, Zhang W, Wang Y, Qian P, Huang H. Inflammation and aging: signaling pathways and intervention therapies. Signal Transduct Target Ther. 2023;8(1):239. doi: 10.1038/s41392-023-01502-8.
43.
Head T, Daunert S, Goldschmidt-Clermont P. The Aging Risk and Atherosclerosis: A Fresh Look at Arterial Homeostasis. Front Genet. 2017;8:216. doi: 10.3389/fgene.2017.00216.
44.
Kuntic M, Kuntic I, Hahad O, Lelieveld J, Münzel T, Daiber A. Impact of air pollution on cardiovascular aging. Mech Ageing Dev. 2023;214:111857. doi: 10.1016/j.mad.2023.111857.
45.
Singam NSV, Fine C, Fleg JL. Cardiac changes associated with vascular aging. Clin Cardiol. 2020;43(2):92–98. doi: 10.1002/clc.23313.
46.
Barodka VM, Joshi BL, Berkowitz DE, Hogue CW Jr, Nyhan D. Review article: implications of vascular aging. Anesth Analg. 2011;112(5):1048–1060. doi: 10.1213/ANE.0b013e3182147e3c.
47.
Pour HA, Norouzzadeh R, Heidari MR. Comparison of Clinical Presentation Related on Risk Factors in Older and Younger Patients with Acute Coronary Syndrome. Int J Clin Cardiol. 2015;2(6). doi: 10.23937/2378-2951/1410058.
48.
Friedman A, Chudow J, Merritt Z, Shulman E, Fisher JD, Ferrick KJ, et al. Electrocardiogram abnormalities in older individuals by race and ethnicity. J Electrocardiol. 2020;63:91–93. doi: 10.1016/j.jelectrocard.2020.09.014.
49.
Xu X, Wang B, Ren C, Hu J, Greenberg DA, Chen T, et al. Recent Progress in Vascular Aging: Mechanisms and Its Role in Age-related Diseases. Aging Dis. 2017;8(4):486–505. doi: 10.14336/AD.2017.0507.
50.
Liu L, Zhao B, Yu Y, Gao W, Liu W, Chen L, et al. Vascular Aging in Ischemic Stroke. J Am Heart Assoc. 2024;13(15):e033341. doi: 10.1161/JAHA.123.033341.
51.
Fonarow GC, Reeves MJ, Zhao X, Olson DM, Smith EE, Saver JL, et al.; Get With the Guidelines-Stroke Steering Committee and Investigators. Age-related differences in characteristics, performance measures, treatment trends, and outcomes in patients with ischemic stroke. Circulation. 2010;121(7):879–891. doi: 10.1161/CIRCULATIONAHA.109.892497.
52.
Li L, Duan L, Xu Y, Ruan H, Zhang M, Zheng Y, et al. Hypertension in frail older adults: current perspectives. PeerJ. 2024;12:e17760. doi: 10.7717/peerj.17760.
53.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al.; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339.
54.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223–237. doi: 10.1038/s41581-019-0244-2.
55.
McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, et al.; ESC Scientific Document Group. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024;45(38):3912–4018. doi: 10.1093/eurheartj/ehae178.
56.
Dent E, Wright ORL, Woo J, Hoogendijk EO. Malnutrition in older adults. Lancet. 2023;401(10380):951–966. doi: 10.1016/S0140-6736(22)02612-5.
57.
Kanda D, Ohishi M. Malnutrition is one of new risk factors in patients with hypertension: the message form Fukushima Cohort Study. Hypertens Res. 2024;47(9):2589–2591. doi: 10.1038/s41440-024-01751-2.
58.
Norman K, Haß U, Pirlich M. Malnutrition in Older Adults-Recent Advances and Remaining Challenges. Nutrients. 2021;13(8):2764. doi: 10.3390/nu13082764.
59.
Chen L, Huang Z, Lu J, Yang Y, Pan Y, Bao K, et al. Impact of the Malnutrition on Mortality in Elderly Patients Undergoing Percutaneous Coronary Intervention. Clin Interv Aging. 2021;16:1347–1356. doi: 10.2147/CIA.S308569.
60.
Arshad S, Khan S, Karim A, Gupta VA. The burden of malnutrition & frailty in patients with coronary artery disease: An under-recognized problem. JRSM Cardiovasc Dis. 2022;11:20480040221102741. doi: 10.1177/20480040221102741.
61.
Wleklik M, Uchmanowicz I, Jankowska-Polańska B, Andreae C, Regulska-Ilow B. The Role of Nutritional Status in Elderly Patients with Heart Failure. J Nutr Health Aging. 2018;22(5):581–588. doi: 10.1007/s12603-017-0985-1.
62.
Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr. 2008;27(1):5–15. doi: 10.1016/j.clnu.2007.10.007.
63.
Volkert D, Beck AM, Cederholm T, Cruz-Jentoft A, Hooper L, Kiesswetter E, et al. ESPEN practical guideline: Clinical nutrition and hydration in geriatrics. Clin Nutr. 2022;41(4):958–989. doi: 10.1016/j.clnu.2022.01.024.
64.
Molfino A, Imbimbo G, Laviano A. Current Screening Methods for the Risk or Presence of Malnutrition in Cancer Patients. Cancer Manag Res. 2022;14:561–567. doi: 10.2147/CMAR.S294105.
65.
Tonet E, Campana R, Caglioni S, Gibiino F, Fiorio A, Chiaranda G, et al. Tools for the Assessment of the Malnutrition Status and Possible Interventions in Elderly with Cardiovascular Diseases. J Clin Med. 2021;10(7):1508. doi: 10.3390/jcm10071508.
66.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al.; ESC Scientific Document Group. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;14(1):111–188. doi: 10.1093/eurheartj/ehz455.
67.
Mortensen MB, Nordestgaard BG. Elevated LDL cholesterol and increased risk of myocardial infarction and atherosclerotic cardiovascular disease in individuals aged 70-100 years: a contemporary primary prevention cohort. Lancet. 2020;396(10263):1644–1652. doi: 10.1016/S0140-6736(20)32233-9.
68.
Gencer B, Marston NA, Im KA, Cannon CP, Sever P, Keech A, et al. Efficacy and safety of lowering LDL cholesterol in older patients: a systematic review and meta-analysis of randomised controlled trials. Lancet. 2020;396(10263):1637–1643. doi: 10.1016/S0140-6736(20)32332-1.
69.
Rozing MP, Westendorp RGJ. Altered cardiovascular risk pattern of LDL cholesterol in older adults. Curr Opin Lipidol. 2023;34(1):22–26. doi: 10.1097/MOL.0000000000000859.
70.
Jamil YA, Cohen R, Alameddine DK, Deo SV, Kumar M, Orkaby AR. Cholesterol Lowering in Older Adults: Should We Wait for Further Evidence? Curr Atheroscler Rep. 2024;26(9):521–536. doi: 10.1007/s11883-024-01224-4.
71.
Chen X, Ding J, Shi Z, Bai K, Shi S, Tian Q. Association of longitudinal trajectories of fasting plasma glucose with all-cause and cardiovascular mortality among a Chinese older population: a retrospective cohort study. BMC Public Health. 2024;24(1):1335. doi: 10.1186/s12889-024-18823-0.
72.
Sinha A, Ning H, Cameron N, Bancks M, Carnethon MR, Allen NB, et al. Atherosclerotic Cardiovascular Disease or Heart Failure: First Cardiovascular Event in Adults With Prediabetes and Diabetes. J Card Fail. 2023;29(3):246–254. doi: 10.1016/j.cardfail.2022.10.426.
73.
Marx N, Federici M, Schütt K, Müller-Wieland D, Ajjan RA, Antunes MJ, et al.; ESC Scientific Document Group. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J. 2023;44(39):4043–4140. doi: 10.1093/eurheartj/ehad192.
74.
Dong XJ, Zhang XQ, Wang BB, Hou FF, Jiao Y. The burden of cardiovascular disease attributable to high fasting plasma glucose: Findings from the global burden of disease study 2019. Diabetes Metab Syndr. 2024;18(5):103025. doi: 10.1016/j.dsx.2024.103025.
75.
Gao Q, Wang Q, Gan Z, Wang M, Lu D, Zhan B. Fasting plasma glucose levels are associated with all-cause and cancer mortality: A population-based retrospective cohort study. PLoS One. 2024;19(11):e0311150. doi: 10.1371/journal.pone.0311150.
76.
Ikegami H, Hiromine Y, Noso S. Insulin-dependent diabetes mellitus in older adults: Current status and future prospects. Geriatr Gerontol Int. 2022;22(8):549–553. doi: 10.1111/ggi.14414.
77.
Araki A. Individualized treatment of diabetes mellitus in older adults. Geriatr Gerontol Int. 2024;24(12):1257–1268. doi: 10.1111/ggi.14979.
78.
Bellary S, Kyrou I, Brown JE, Bailey CJ. Type 2 diabetes mellitus in older adults: clinical considerations and management. Nat Rev Endocrinol. 2021;17(9):534–548. doi: 10.1038/s41574-021-00512-2.
79.
Xue M, Xu W, Ou YN, Cao XP, Tan MS, Tan L, et al. Diabetes mellitus and risks of cognitive impairment and dementia: A systematic review and meta-analysis of 144 prospective studies. Ageing Res Rev. 2019;55:100944. doi: 10.1016/j.arr.2019.100944.
80.
Yun JS, Kim K, Ahn YB, Han K, Ko SH. Holistic and Personalized Strategies for Managing in Elderly Type 2 Diabetes Patients. Diabetes Metab J. 2024;48(4):531–545. doi: 10.4093/dmj.2024.0310.
81.
Anagnostis P, Gkekas NK, Achilla C, Pananastasiou G, Taouxidou P, Mitsiou M, et al. Type 2 Diabetes Mellitus is Associated with Increased Risk of Sarcopenia: A Systematic Review and Meta-analysis. Calcif Tissue Int. 2020;107(5):453–463. doi: 10.1007/s00223-020-00742-y.
82.
Sinclair A, Morley J. Frailty and diabetes. Lancet. 2013;382(9902):1386–1387. doi: 10.1016/S0140-6736(13)61676-1.
83.
Orkaby AR, Onuma O, Qazi S, Gaziano JM, Driver JA. Preventing cardiovascular disease in older adults: One size does not fit all. Cleve Clin J Med. 2018;85(1):55–64. doi: 10.3949/ccjm.85a.16119.
84.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al.; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156. doi: 10.1093/gerona/56.3.m146.
85.
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–727. doi: 10.1093/gerona/62.7.722.
86.
Shamsalinia A, Hosseini SR, Bijani A, Ghadimi R, Saadati K, Kordbageri MR, et al. Cardiovascular disease risk factors and frailty syndrome in community-dwelling older adults: Results from the Amirkola Health and Aging Project Cohort Study. BMC Geriatr. 2024;24(1):665. doi: 10.1186/s12877-024-05268-8.
87.
James K, Jamil Y, Kumar M, Kwak MJ, Nanna MG, Qazi S, et al. Frailty and Cardiovascular Health. J Am Heart Assoc. 2024;13(15):e031736. doi: 10.1161/JAHA.123.031736.
88.
Joyce E. Frailty and cardiovascular disease: A two-way street? Cleve Clin J Med. 2018;85(1):65–68. doi: 10.3949/ccjm.85a.17075.
89.
Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, et al. Cardiovascular Risks Associated with Gender and Aging. J Cardiovasc Dev Dis. 2019;6(2):19. doi: 10.3390/jcdd6020019.
90.
Prell T, Grimm A, Axer H. Uncovering sarcopenia and frailty in older adults by using muscle ultrasound-A narrative review. Front Med (Lausanne). 2024;11:1333205. doi: 10.3389/fmed.2024.1333205.
91.
Damluji AA, Alfaraidhy M, AlHajri N, Rohant NN, Kumar M, Al Malouf C, et al. Sarcopenia and Cardiovascular Diseases. Circulation. 2023;147(20):1534–1553. doi: 10.1161/CIRCULATIONAHA.123.064071.
92.
Zuo X, Li X, Tang K, Zhao R, Wu M, Wang Y, et al. Sarcopenia and cardiovascular diseases: A systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2023;14(3):1183–1198. doi: 10.1002/jcsm.13221.
93.
Dunlay SM, Chamberlain AM. Multimorbidity in Older Patients with Cardiovascular Disease. Curr Cardiovasc Risk Rep. 2016;10:3. doi: 10.1007/s12170-016-0491-8.
94.
Aïdoud A, Gana W, Poitau F, Debacq C, Leroy V, Nkodo JA, et al. High Prevalence of Geriatric Conditions Among Older Adults With Cardiovascular Disease. J Am Heart Assoc. 2023;12(2):e026850. doi: 10.1161/JAHA.122.026850.
95.
Forman DE, Maurer MS, Boyd C, Brindis R, Salive ME, McFarland Horne F, et al. Multimorbidity in Older Adults With Cardiovascular Disease. J Am Coll Cardiol. 2018;71(19):2149–2161. doi: 10.1016/j.jacc.2018.03.022.
96.
Chen LJ, Sha S, Brenner H, Schöttker B. Longitudinal associations of polypharmacy and frailty with major cardiovascular events and mortality among more than half a million middle-aged participants of the UK Biobank. Maturitas. 2024;185:107998. doi: 10.1016/j.maturitas.2024.107998.
97.
Canio WC. Polypharmacy in Older Adults. Clin Geriatr Med. 2022;38(4):621–625. doi: 10.1016/j.cger.2022.05.004.
98.
Thompson W, McDonald EG. Polypharmacy and Deprescribing in Older Adults. Annu Rev Med. 2024;75:113–127. doi: 10.1146/annurev-med-070822-101947.
99.
Nagar S, Ma L, Pan Y, Huynh ALH, Tan ECK, Jin L. A need to integrate pharmacological management for multimorbidity into dementia guidelines in Australia. Front Public Health. 2024;12:1425195. doi: 10.3389/fpubh.2024.1425195.
100.
van Poelgeest E, Seppala L, Bahat G, Ilhan B, Mair A, van Marum R, et al.; EuGMS SIG Pharmacology. Optimizing pharmacotherapy and deprescribing strategies in older adults living with multimorbidity and polypharmacy: EuGMS SIG on pharmacology position paper. Eur Geriatr Med. 2023;14(6):1195–1209. doi: 10.1007/s41999-023-00872-0.
101.
Triantafyllou A, Douma S. Cardiovascular risk assessment in elderly individuals without overt CVD disease. Could traditional risk factors fit in all ages? J Clin Hypertens (Greenwich). 2019;21(8):1153–1154. doi: 10.1111/jch.13616.
102.
Bambrick P, Tan WS, Mulcahy R, Pope GA, Cooke J. Vascular risk assessment in older adults without a history of cardiovascular disease. Exp Gerontol. 2016;79:37–45. doi: 10.1016/j.exger.2016.03.002.
103.
Żurański W, Nowak J, Danikiewicz A, Zubelewicz-Szkodzińska B, Hudzik B. Assessing Cardiovascular Risk in Geriatric Patients Without Atherosclerotic Cardiovascular Disease. J Clin Med. 2024;13(23):7133. doi: 10.3390/jcm13237133.
104.
SCORE2-OP working group and ESC Cardiovascular risk collaboration. SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur Heart J. 2021;42(25):2455–2467. doi: 10.1093/eurheartj/ehab312.
105.
van Trier TJ, Snaterse M, Boekholdt SM, Scholte Op Reimer WJ, Hageman SH, Visseren FL, et al. Validation of Systematic Coronary Risk Evaluation 2 (SCORE2) and SCORE2-Older Persons in the EPIC-Norfolk prospective population cohort. Eur J Prev Cardiol. 2024;31(2):182–189. doi: 10.1093/eurjpc/zwad318.
106.
Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ. 2017;357:j2099. doi: 10.1136/bmj.j2099.
107.
Strandberg TE. Challenges of treating cardiovascular risk in old age. Lancet Healthy Longev. 2021;2(6):e308–e309. doi: 10.1016/S2666-7568(21)00114-8.
108.
Manuel DG, Tuna M, Bennett C, Hennessy D, Rosella L, Sanmartin C, et al. Development and validation of a cardiovascular disease risk-prediction model using population health surveys: the Cardiovascular Disease Population Risk Tool (CVDPoRT). CMAJ. 2018;190(29):E871–E882. doi: 10.1503/cmaj.170914.
109.
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB Sr, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2935–2959. doi: 10.1016/j.jacc.2013.11.005.
110.
WHO CVD Risk Chart Working Group. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332–e1345. doi: 10.1016/S2214-109X(19)30318-3.
111.
Mortensen MB, Fuster V, Muntendam P, Mehran R, Baber U, Sartori S, et al. Negative Risk Markers for Cardiovascular Events in the Elderly. J Am Coll Cardiol. 2019;74(1):1–11. doi: 10.1016/j.jacc.2019.04.049.
112.
Kasim SS, Ibrahim N, Malek S, Ibrahim KS, Aziz MF, Song C, et al. Validation of the general Framingham Risk Score (FRS), SCORE2, revised PCE and WHO CVD risk scores in an Asian population. Lancet Reg Health West Pac. 2023;35:100742. doi: 10.1016/j.lanwpc.2023.100742.
113.
Nanna MG, Abdullah A, Mortensen MB, Navar AM. Primary prevention statin therapy in older adults. Curr Opin Cardiol. 2023;38(1):11–20. doi: 10.1097/HCO.0000000000001003.
114.
Houghton JSM, Saratzis AN, Sayers RD, Haunton VJ. New Horizons in Peripheral Artery Disease. Age Ageing. 2024;53(6):afae114. doi: 10.1093/ageing/afae114.
115.
Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, et al.; PROSPER study group. PROspective Study of Pravastatin in the Elderly at Risk. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360(9346):1623–1630. doi: 10.1016/s0140-6736(02)11600-x.
116.
Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M, et al.; ASCOT Investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Drugs. 2004;64 Suppl 2:43–60. doi: 10.2165/00003495-200464002-00005.
117.
Glynn RJ, Koenig W, Nordestgaard BG, Shepherd J, Ridker PM. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Ann Intern Med. 2010;152(8):488–496, W174. doi: 10.7326/0003-4819-152-8-201004200-00005.
118.
Al-Ani A, Jamil Y, Orkaby AR. Treating Hypercholesterolemia in Older Adults for Primary Prevention of Cardiovascular Events. Drugs Aging. 2024;41(9):699–712. doi: 10.1007/s40266-024-01139-4.
119.
Parr E, Ferdinand P, Roffe C. Management of Acute Stroke in the Older Person. Geriatrics (Basel). 2017;2(3):27. doi: 10.3390/geriatrics2030027.
120.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. doi: 10.1161/CIR.0000000000000678.
121.
Mangione CM, Barry MJ, Nicholson WK, Cabana M, Chelmow D, Coker TR, et al. Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2022;328(8):746–753. doi: 10.1001/jama.2022.13044.
122.
Hennekens CH, Desai AS, Bandi R, Bonthu S, Pfeffer MA, Ferris AH. New Clinical Challenges for Health Providers in the Prescription of Statins in the Elderly. Am J Med. 2024;137(3):189–191. doi: 10.1016/j.amjmed.2023.11.014.
123.
Pragmatic Evaluation of Events and Benefits of Lipid-lowering in Older Adults (PREVENTABLE). ClinicalTrials.gov [online] https://www.clinicaltrials.gov... [accessed on 16 October 2023]. Statins in Reducing events in the Elderly (STAREE) Heart Sub-study (STAREE-HEART). ClinicalTrials.gov [online] https://clinicaltrials.gov/stu... [accessed on 16 October 2023].
124.
Statins in Reducing events in the Elderly (STAREE) Heart Sub-study (STAREE-HEART). ClinicalTrials.gov [online] https://clinicaltrials.gov/stu... [accessed on 16 October 2023].
Share
RELATED ARTICLE
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.