Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Analysis of echocardiographic parameters suggestive of pulmonary hypertension in patients with heart failure with preserved ejection fraction and assessment of clinical features favoring development of the PH-phenotype
1
1st Department of Cardiology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland; European Reference Network for Rare and Low Prevalence Complex Diseases of the Heart (ERN GUARD-Heart)
Corresponding author
Julia Dołęga
Klinika Kardiologii I Katedry Kardiologii, Śląski Uniwersytet Medyczny w Katowicach, ul. Ziołowa 47, 40-635 Katowice
Klinika Kardiologii I Katedry Kardiologii, Śląski Uniwersytet Medyczny w Katowicach, ul. Ziołowa 47, 40-635 Katowice
Ann. Acad. Med. Siles. 2025;79:92-100
KEYWORDS
heart failureheart failure with preserved ejection fractionpostcapillary pulmonary hypertensionchronic atrial fibrillation
TOPICS
ABSTRACT
Introduction:
Heart failure with preserved ejection fraction (HFpEF) is characterized by left ventricle (LV) diastolic dysfunction. Impaired diastolic function induces pulmonary congestion and leads to postcapillary pulmonary hypertension (PH), which is an important contributor to clinical deterioration and increased mortality.
Material and methods:
A retrospective one-centre analysis of 63 consecutive patients hospitalized due to HFpEF was performed. The study group was divided according to the echocardiographic probability of PH using tricuspid regurgitation peak velocity (TRV) into two groups: TRV ≥ 2.8 m/s – with an increased probability of PH (n = 15 (23.8%); females: 3 (20%); mean age 72.7 ± 10.8) and TRV < 2.8 m/s – with a low probability of PH (n = 48 (76.2%); females: 25 (52.1%); mean age 72.3 ± 13.7). The clinical data, transthoracic echocardiography (TTE) parameters and laboratory tests were analyzed.
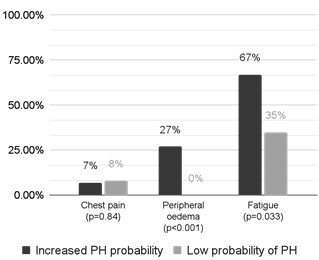
Results:
The group of patients with an increased probability of PH was characterized by more severe HF symptoms, more frequent fatigue (p = 0.03) and the occurrence of ankle swelling (p < 0.01). Analysis of the baseline data revealed a trend towards a greater incidence of atrial fibrillation (AF; p = 0.08) in this group. The patients who had TRV ≥ 2.8 m/s had a larger left atrial area (p < 0.001), a higher E/A ratio (p < 0.001) with borderline differences in the left ventricular mass index (LVMI; p = 0.06) and left ventricular ejection fraction (LVEF; p = 0.07).
Conclusions:
About 25% of patients with HFpEF, mostly males, present with moderate features of PH that are associated with more advanced LV and left atrium (LA) remodeling and dysfunction. However, they are not reflected in the classic comorbidities, with the exception of AF.
Heart failure with preserved ejection fraction (HFpEF) is characterized by left ventricle (LV) diastolic dysfunction. Impaired diastolic function induces pulmonary congestion and leads to postcapillary pulmonary hypertension (PH), which is an important contributor to clinical deterioration and increased mortality.
Material and methods:
A retrospective one-centre analysis of 63 consecutive patients hospitalized due to HFpEF was performed. The study group was divided according to the echocardiographic probability of PH using tricuspid regurgitation peak velocity (TRV) into two groups: TRV ≥ 2.8 m/s – with an increased probability of PH (n = 15 (23.8%); females: 3 (20%); mean age 72.7 ± 10.8) and TRV < 2.8 m/s – with a low probability of PH (n = 48 (76.2%); females: 25 (52.1%); mean age 72.3 ± 13.7). The clinical data, transthoracic echocardiography (TTE) parameters and laboratory tests were analyzed.
Results:
The group of patients with an increased probability of PH was characterized by more severe HF symptoms, more frequent fatigue (p = 0.03) and the occurrence of ankle swelling (p < 0.01). Analysis of the baseline data revealed a trend towards a greater incidence of atrial fibrillation (AF; p = 0.08) in this group. The patients who had TRV ≥ 2.8 m/s had a larger left atrial area (p < 0.001), a higher E/A ratio (p < 0.001) with borderline differences in the left ventricular mass index (LVMI; p = 0.06) and left ventricular ejection fraction (LVEF; p = 0.07).
Conclusions:
About 25% of patients with HFpEF, mostly males, present with moderate features of PH that are associated with more advanced LV and left atrium (LA) remodeling and dysfunction. However, they are not reflected in the classic comorbidities, with the exception of AF.
REFERENCES (22)
1.
Eltelbany M., Shah P., deFilippi C. Biomarkers in HFpEF for diagnosis, prognosis, and biological phenotyping. Curr. Heart Fail. Rep. 2022; 19(6): 412–424, doi: 10.1007/s11897-022-00578-7.
2.
Chen Y., Guo H., Xu D., Xu X., Wang H., Hu X. et al. Left ventricular failure produces profound lung remodeling and pulmonary hypertension in mice: heart failure causes severe lung disease. Hypertension 2012; 59(6): 1170–1178, doi: 10.1161/HYPERTENSIONAHA.111.186072.
3.
Karasek D., Sinkiewicz W. Nadciśnienie płucne w przebiegu chorób lewego serca — aktualne leczenie i kierunki rozwoju terapii. Folia Cardiol. 2017; 12(3): 317–325, doi: 10.5603/FC.2017.0061.
4.
Rosenkranz S., Gibbs J.S.R., Wachter R., De Marco T., Vonk-Noordegraaf A., Vachiéry J.L. Left ventricular heart failure and pulmonary hypertension. Eur. Heart J. 2016; 37(12): 942–954, doi: 10.1093/eurheartj/ehv512.
5.
Melenovsky V., Hwang S.J., Lin G., Redfield M.M., Borlaug B.A. Right heart dysfunction in heart failure with preserved ejection fraction. Eur. Heart J. 2014; 35(48): 3452–3462, doi: 10.1093/eurheartj/ehu193.
6.
Humbert M., Kovacs G., Hoeper M.M., Badagliacca R., Berger R.M.F., Brida M. et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur. Heart J. 2022; 43(38): 3618–3731, doi: 10.1093/eurheartj/ehac237. Erratum in: Eur. Heart J. 2023; 44(15): 1312, doi: 10.1093/eurheartj/ehad005.
7.
Corrigendum to: 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: Developed by the task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). Endorsed by the International Society for Heart and Lung Transplantation (ISHLT) and the European Reference Network on rare respiratory diseases (ERN-LUNG). Eur. Heart J. 2023; 44(15): 1312, doi: 10.1093/eurheartj/ehad005. Erratum for: Eur. Heart J. 2022; 43(38): 3618–3731, doi: 10.1093/eurheartj/ehac237.
8.
Pieske B., Tschöpe C., de Boer R.A., Fraser A.G., Anker S.D., Donal E. et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. Heart J. 2019; 40(40): 3297–3317, doi: 10.1093/eurheartj/ehz641. Erratum in: Eur. Heart J. 2021; 42(13): 1274, doi: 10.1093/eurheartj/ehaa1016.
9.
McDonagh T.A., Metra M., Adamo M., Gardner R.S., Baumbach A., Böhm M. et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2024; 26(1): 5–17, doi: 10.1002/ejhf.3024.
10.
Humbert M., Kovacs G., Hoeper M.M., Badagliacca R., Berger R.M.F., Brida M. et al. Wytyczne ESC/ERS 2022 dotyczące rozpoznawania i leczenia nadciśnienia płucnego. Polskie Towarzystwo Kardiologiczne, 2023-06-13 [online] https://ptkardio.pl/wytyczne/4... [accessed on 3 December 2024].
11.
Hindricks G., Potpara T., Dagres N., Arbelo E., Bax J.J., Blom-ström‑Lundqvist C. et al. Wytyczne ESC 2020 dotyczące diagnostyki i leczenia migotania przedsionków opracowane we współpracy z European Association of Cardio‑Thoracic Surgery (EACTS). Polskie Towarzystwo Kardiologiczne, 2021-03-04 [online] https://ptkardio.pl/resources/... [accessed on 3 December 2024].
12.
Abd-El-Aziz T.A. Noninvasive prediction of left ventricular end-diastolic pressure in patients with coronary artery disease and preserved ejection fraction. Can. J. Cardiol. 2012; 28(1): 80–86, doi: 10.1016/j.cjca.2011.02.001.
13.
Shah A.M., Cikes M., Prasad N., Li G., Getchevski S., Claggett B. et al. Echocardiographic features of patients with heart failure and preserved left ventricular ejection fraction. J. Am. Coll. Cardiol. 2019; 74(23): 2858–2873, doi: 10.1016/j.jacc.2019.09.063.
14.
Shah A.M., Shah S.J., Anand I.S., Sweitzer N.K., O’Meara E., Heitner J.F. et al. Cardiac structure and function in heart failure with preserved ejection fraction: baseline findings from the echocardiographic study of the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist trial. Circ. Heart Fail. 2014; 7(1): 104–115, doi: 10.1161/CIRCHEARTFAILURE.113.000887.
15.
Lam C.S., Roger V.L., Rodeheffer R.J., Borlaug B.A., Enders F.T., Redfield M.M. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J. Am. Coll. Cardiol. 2009; 53(13): 1119–1126, doi: 10.1016/j.jacc.2008.11.051.
16.
Leung C.C., Moondra V., Catherwood E., Andrus B.W. Prevalence and risk factors of pulmonary hypertension in patients with elevated pulmonary venous pressure and preserved ejection fraction. Am. J. Cardiol. 2010; 106(2): 284–286, doi: 10.1016/j.amjcard.2010.02.039.
17.
Obokata M., Reddy Y.N.V., Pislaru S.V., Melenovsky V., Borlaug B.A. Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation 2017; 136(1): 6–19, doi: 10.1161/CIRCULATIONAHA.116.026807.
18.
Shah A.M. Ventricular remodeling in heart failure with preserved ejection fraction. Curr. Heart Fail. Rep. 2013; 10(4): 341–349, doi: 10.1007/s11897-013-0166-4.
19.
Santos A.B., Kraigher-Krainer E., Gupta D.K., Claggett B., Zile M.R., Pieske B. et al. Impaired left atrial function in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2014; 16(10): 1096–1103, doi: 10.1002/ejhf.147.
20.
Freed B.H., Daruwalla V., Cheng J.Y., Aguilar F.G., Beussink L., Choi A. et al. Prognostic utility and clinical significance of cardiac mechanics in heart failure with preserved ejection fraction: importance of left atrial strain. Circ. Cardiovasc. Imaging 2016; 9(3), doi: 10.1161/CIRCIMAGING.115.003754.
21.
Rabkin S.W. Evaluating the adverse outcome of subtypes of heart failure with preserved ejection fraction defined by machine learning: A systematic review focused on defining high risk phenogroups. EXCLI J. 2022; 21: 487–518, doi: 10.17179/excli2021-4572.
22.
Tan Y.T., Wenzelburger F., Lee E., Heatlie G., Leyva F., Patel K. et al. The pathophysiology of heart failure with normal ejection fraction: exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion. J. Am. Coll. Cardiol. 2009; 54(1): 36–46, doi: 10.1016/j.jacc.2009.03.037.
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.