Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Hidden umbilical anomalies: case reports of newborns with a persistent urachus and a persistent vitellointestinal duct
1
Students’ Scientific Club at the Department of Paediatric Surgery and Urology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
2
Department of Paediatric Surgery and Urology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
Corresponding author
Aleksandra Kątnik
Studenckie Koło Naukowe, Klinika Chirurgii i Urologii Dziecięcej, SPSK Nr 6 ŚUM Górnośląskie Centrum Zdrowia Dziecka im. Jana Pawła II, ul. Medyków 16, 40-752 Katowice
Studenckie Koło Naukowe, Klinika Chirurgii i Urologii Dziecięcej, SPSK Nr 6 ŚUM Górnośląskie Centrum Zdrowia Dziecka im. Jana Pawła II, ul. Medyków 16, 40-752 Katowice
Ann. Acad. Med. Siles. 2025;79:101-105
KEYWORDS
umbilical fistulaomphalomesenteric duct remnantpatent vitellointestinal ductcongenital malformationspatent urachus
TOPICS
ABSTRACT
Introduction:
Anomalies in the umbilical region of newborns encompass a range of congenital malformations that require careful diagnosis. These conditions may lead to delayed healing of the umbilical stump, discharge from the navel, and pose challenges for pediatricians. Among these, vitellointestinal duct (VID) anomalies are the most common, occurring in approximately 2–3% of the population. The VID, an embryonic structure connecting the yolk sac to the primitive midgut, normally regresses during development. Failure of this process can result in various anomalies, the most common being Meckel’s diverticulum. Similarly, urachal anomalies arise when embryonic urachus persists, potentially presenting as abnormalities at the umbilicus.
Case reports:
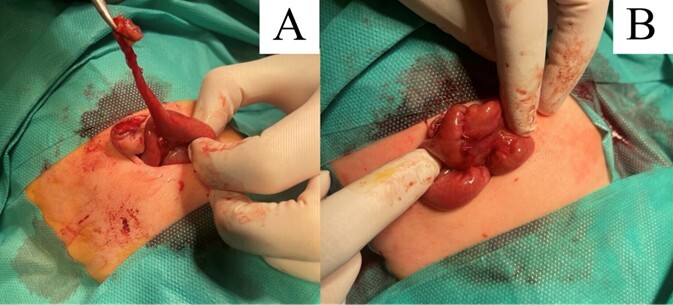
A 6-day-old male newborn with a draining fistula at the umbilicus was transferred to our institution with a suspected diagnosis of persistent urachus. After admission, the visible fistula was catheterized under ultrasound guidance, revealing a connection to the intestinal loops. This finding indicated a diagnosis of a persistent VID, which was subsequently excised. Another patient was a 15-day-old female newborn with a bladder defect detected during a prenatal ultrasound examination. An everted patent urachus was diagnosed after birth, which was subsequently treated by means of surgical excision.
Conclusions:
Abnormalities in the umbilicus may raise the suspicion of persistent fetal structures. A thorough physical examination, supplemented by ultrasound and catheterization, can effectively make the correct diagnosis. Surgical treatment is recommended, involving resection of the persistent urachus or resection of the persistent VID with the bowel fragment.
Anomalies in the umbilical region of newborns encompass a range of congenital malformations that require careful diagnosis. These conditions may lead to delayed healing of the umbilical stump, discharge from the navel, and pose challenges for pediatricians. Among these, vitellointestinal duct (VID) anomalies are the most common, occurring in approximately 2–3% of the population. The VID, an embryonic structure connecting the yolk sac to the primitive midgut, normally regresses during development. Failure of this process can result in various anomalies, the most common being Meckel’s diverticulum. Similarly, urachal anomalies arise when embryonic urachus persists, potentially presenting as abnormalities at the umbilicus.
Case reports:
A 6-day-old male newborn with a draining fistula at the umbilicus was transferred to our institution with a suspected diagnosis of persistent urachus. After admission, the visible fistula was catheterized under ultrasound guidance, revealing a connection to the intestinal loops. This finding indicated a diagnosis of a persistent VID, which was subsequently excised. Another patient was a 15-day-old female newborn with a bladder defect detected during a prenatal ultrasound examination. An everted patent urachus was diagnosed after birth, which was subsequently treated by means of surgical excision.
Conclusions:
Abnormalities in the umbilicus may raise the suspicion of persistent fetal structures. A thorough physical examination, supplemented by ultrasound and catheterization, can effectively make the correct diagnosis. Surgical treatment is recommended, involving resection of the persistent urachus or resection of the persistent VID with the bowel fragment.
REFERENCES (20)
1.
Hegazy A.A. Anatomy and embryology of umbilicus in newborns: a review and clinical correlations. Front. Med. 2016; 10(3): 271–277, doi: 10.1007/s11684-016-0457-8.
2.
Rege S.A., Saraf V.B., Jadhav M. Persistent omphalomesenteric duct and urachus presenting as an umbilical hernia. BMJ Case Rep. 2022; 15(4): e247789, doi: 10.1136/bcr-2021-247789.
3.
Wilson A.L., Gandhi J., Seyam O., Rahmani B., Patel S., Joshi G. et al. Urachal anomalies: A review of pathological conditions, diagnosis, and management. Transl. Res. Anat. 2019; 16: 100041, doi: 10.1016/j.tria.2019.100041.
4.
Walia D.S., Singla A., Singla D., Kaur R. Patent vitellointestinal duct with patent urachus presenting as umbilical discharge. J. Clin. Diagn. Res. 2017; 11(3): PD01, doi: 10.7860/JCDR/2017/24726.9366.
5.
Inarejos Clemente E.J., Navarro O.M., Navallas Irujo M., Ladera E., Colombo C., Suñol M. et al. Omphalomesenteric duct anomalies in children: A multimodality overview. Radiographics 2021; 41(7): 2090–2110, doi: 10.1148/rg.2021210048.
6.
Ayyanar P., Tripathy B.B., Pati A.B., Mohanty M.K., Sable M. Ectopic pancreas, gastric, duodenal and colonic tissue in a case of persistent umbili-cal discharge: Report of two patients with review of literature. Indian J. Pathol. Microbiol. 2023; 66(2): 403–406, doi: 10.4103/ijpm.ijpm_526_21.
7.
Hawariat B.Y.W., Ali A.O., Gebreselassie H.A. Ileal prolapse through patent omphalomesenteric duct in a two year-old boy: a case report. J. Med. Case Rep. 2024; 18(1): 67, doi: 10.1186/s13256-024-04370-0.
8.
Tamilselvan K., Mohan A., Cheslyn-Curtis S., Eisenhut M. Persistent umbilical discharge from an omphalomesenteric duct cyst containing gastric mucosa. Case Rep. Pediatr. 2012; 2012: 482185, doi: 10.1155/2012/482185.
9.
Tawk A., Abdallah A., Meouchy P., Salameh J., Khoury S., Kyriakos M. et al. Omphalitis with umbilical abscess in an adult with a urachal remnant. Case Rep. Gastroenterol. 2021; 15(3): 966–971, doi: 10.1159/000518870.
10.
Yoneda A., Hida T., Tetsuo H., Fukui S., Murakami S., Miyoshi T. et al. A case of retroperitoneal abscess caused by infection of urachal remnant. Clin. Case Rep. 2022; 10(4): e05750, doi: 10.1002/ccr3.5750.
11.
Van Breusegem P., Verswijvel G., Fransis S., Van der Speeten K. Peritoneal surface malignancies originating from urachal carcinoma: case reports and review of the literature. Indian J. Surg. Oncol. 2023; 14(Suppl 1): 109–121, doi: 10.1007/s13193-022-01679-4.
12.
Karakas C., Katzman P.J., Wakeman D.S., Chacon M. Umbilical appendix masquerading as a patent omphalomesenteric duct in a neonate. Pediatr. Dev. Pathol. 2022; 25(4): 474–478, doi: 10.1177/10935266221078500.
13.
Chien C.W., Chen K.J., Lai J.Y., Chao A.S. Patent urachus or bladder exstrophy occulta? A case of prenatally disappeared umbilical cord cyst. Urol. Case Rep. 2021; 39: 101772, doi: 10.1016/j.eucr.2021.101772.
14.
Arlen A.M., Smith E.A. Disorders of the bladder and cloacal anomaly. Clin. Perinatol. 2014; 41(3): 695–707, doi: 10.1016/j.clp.2014.05.015.
15.
Falke G.F., Gonzalez S.T., Berberian L., Marchionatti S., Heredia S., Salomon A. et al. Congenital bladder prolapse through a patent urachus: two institutions’ experience. Urology 2021; 149: e1–e4, doi: 10.1016/j.urology.2020.12.026.
16.
Miyao M., Takahashi T., Uchida E. A case of anomalous congenital band that was difficult to differentiate from omphalomesenteric duct anomaly. J. Nippon Med. Sch. 2017; 84(6): 304–307, doi: 10.1272/jnms.84.304.
17.
Kang A., Kim S.H., Cho Y.H., Kim H.Y. Surgical perspectives of symptomatic omphalomesenteric duct remnants: Differences between infancy and beyond. World J. Clin. Cases 2021; 9(36): 11228–11236, doi: 10.12998/wjcc.v9.i36.11228.
18.
Durakbasa C.U., Okur H., Mutus H.M., Bas A., Ozen M.A., Sehiralti V. et al. Symptomatic omphalomesenteric duct remnants in children. Pediatr. Int. 2010; 52(3): 480–484, doi: 10.1111/j.1442-200X.2009.02980.x.
19.
Azhar M., Zamir N., Taqvi S.R., Shaikh M. Spectrum of omphalomesenteric duct related anomalies and their surgical management in children. Cureus 2021; 13(3): e13898, doi: 10.7759/cureus.13898.
20.
Cilento B.G. Jr, Bauer S.B., Retik A.B., Peters C.A., Atala A. Urachal anomalies: defining the best diagnostic modality. Urology 1998; 52(1): 120–122, doi: 10.1016/s0090-4295(98)00161-7.
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.