Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
High-flow nasal oxygen therapy used to facilitate bronchofiberoscopy in high-risk patients not qualified for urgent bronchofiberoscopy procedure
1
Department of Lung Diseases and Tuberculosis, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland
Corresponding author
Aleksandra Oraczewska
Katedra i Klinika Chorób Płuc i Gruźlicy, Wydział Nauk Medycznych w Zabrzu ŚUM, ul. Koziołka 1, 41-803 Zabrze
Katedra i Klinika Chorób Płuc i Gruźlicy, Wydział Nauk Medycznych w Zabrzu ŚUM, ul. Koziołka 1, 41-803 Zabrze
Ann. Acad. Med. Siles. 2025;79:231-236
KEYWORDS
TOPICS
ABSTRACT
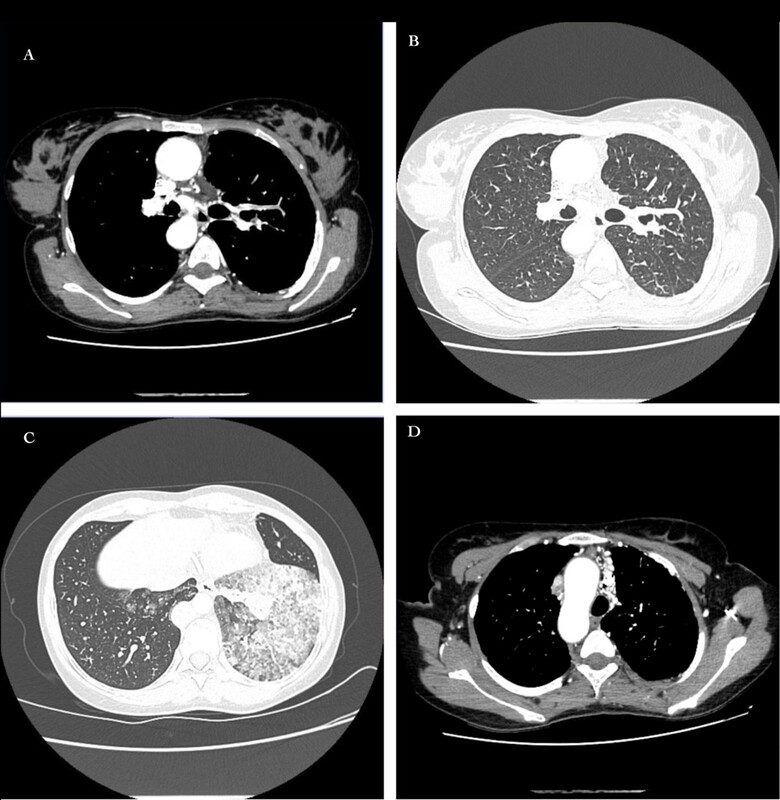
The case series illustrates clinical challenges associated with performing fiberoptic bronchoscopy (FOB) on patients with severe respiratory and cardiovascular diseases. Standard respiratory support methods may be insufficient or may pose risks in this population. The first case involved a patient with a congenital heart defect, unstable hemodynamics, and suspected inflammatory changes in the lungs who required diagnostic FOB due to bleeding from the respiratory tract. Use of high-flow nasal oxygen therapy (HFNOT) allowed for safe performance of FOB, minimizing the risk of barotrauma-related complications. The second patient was diagnosed with Melnick-Needles syndrome, chronic respiratory failure and bronchial cartilage chondromalacia, which can be responsible for complications during standard FOB. HFNOT was also used during the procedure, which prevented complications resulting from anatomical limitations and barotrauma. These cases suggest that HFNOT is an effective alternative to traditional respiratory support methods during FOB for patients at a high risk of complications, especially those with congenital heart defector airway anomalies.
FUNDING
The research was performed as a part of the Medical University of Silesia grant No. BNW-1-105/N/5/K.
CONFLICT OF INTEREST
There was no conflict of interest.
REFERENCES (8)
1.
Shioji N., Kanazawa T., Iwasaki T., Shimizu K., Suemori T., Kuroe Y. et al. High-flow nasal cannula versus noninvasive ventilation for postextubation acute respiratory failure after pediatric cardiac surgery. Acta Med. Okayama 2019; 73(1): 15–20, doi: 10.18926/AMO/56454.
2.
Elmitwalli I., Abdelhady E., Kalsotra S., Gehred A., Tobias J.D., Olbrecht V.A. Use of high-flow nasal cannula versus other noninvasive ventilation techniques or conventional oxygen therapy for respiratory support following pediatric cardiac surgery: A systematic review and meta-analysis. Paediatr. Anaesth. 2024; 34(6): 519–531, doi: 10.1111/pan.14866.
3.
Duan X., Wei N., Wei J., Zhu Y., Kang Y., He Y. et al. Effect of high-flow nasal cannula oxygen therapy on pediatric patients with congenital heart disease in procedural sedation: A prospective, randomized trial. J. Cardiothorac. Vasc. Anesth. 2021; 35(10): 2913–2919, doi: 10.1053/j.jvca.2021.03.031.
4.
Masip J., Peacock W.F., Price S., Cullen L., Martin-Sanchez F.J., Seferovic P. et al. Indications and practical approach to non-invasive ventilation in acute heart failure. Eur. Heart J. 2018; 39(1): 17–25, doi: 10.1093/eurheartj/ehx580.
5.
Oh C.H., Lee C.H., Kim S.Y., Lee S.Y., Jun H.H., Lee S. A family of Melnick-Needles syndrome: a case report. BMC Pediatr. 2020; 20(1): 391, doi: 10.1186/s12887-020-02288-2.
6.
Santos H.H., Garcia P.P., Pereira L., Leão L.L., Aguiar R.A., Lana A.M. et al. Mutational analysis of two boys with the severe perinatally lethal Melnick-Needles syndrome. Am. J. Med. Genet. A 2010; 152A(3): 726–731, doi: 10.1002/ajmg.a.33260.
7.
Oraczewska A., Cofta S., Warcholiński A., Trejnowska E., Brożek G., Swinarew A. et al. The use of non-invasive respiratory assistance to facilitate bronchofiberoscopy performance in patients with hypoxemic (type 1) respiratory failure – study protocol. Adv. Med. Sci. 2023; 68(2): 474–481, doi: 10.1016/j.advms.2023.10.011.
8.
Wu Q., Xiang G., Song J., Xie L., Wu X., Hao S. et al. Effects of non-invasive ventilation in subjects undergoing cardiac surgery on length of hospital stay and cardiac-pulmonary complications: a systematic review and meta-analysis. J. Thorac. Dis. 2020; 12(4): 1507–1519, doi: 10.21037/jtd.2020.02.30.
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.