Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Fiberoptic bronchoscopy supported with HFNC/NIV as promising management in patients with high risk of respiratory failure
1
Students’ Scientific Club, Department of Lung Diseases and Tuberculosis, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland
2
Department of Lung Diseases and Tuberculosis, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland
3
Department of Anesthesiology and Intensive Therapy, Sergeant Grzegorz Załoga Independent Public Health Care Institute of the Ministry of Internal Affairs and Administration in Katowice, Poland
Corresponding author
Szymon Gawęda
Studenckie Koło Naukowe przy Katedrze i Klinice Chorób Płuc i Gruźlicy, Śląski Uniwersytet Medyczny w Katowicach
Studenckie Koło Naukowe przy Katedrze i Klinice Chorób Płuc i Gruźlicy, Śląski Uniwersytet Medyczny w Katowicach
Ann. Acad. Med. Siles. 2024;78:317-323
KEYWORDS
fiberoptic bronchoscopynon-invasive ventilationhigh-flow nasal cannulaairways diagnosticsrespiratory failure
TOPICS
ABSTRACT
Introduction:
Fiberoptic bronchoscopy (FOB) is a minimally invasive procedure which improves diagnostics and therapeutic management in patients with lung-related conditions. Although it is a generally well-tolerated intervention and there are only few contraindications for FOB, it has to be acknowledged that it causes acute narrowing of the airways and patients with inadequate oxygenation and respiratory acidosis may be disqualified from bronchoscopy due to an increased risk of respiratory failure (RF) development. Noninvasive techniques such as a high-flow nasal cannula (HFNC) and non-invasive ventilation (NIV) are accepted methods of respiratory support in patients with RF, however, their usage in patients undergoing FOB is still poorly represented in the literature.
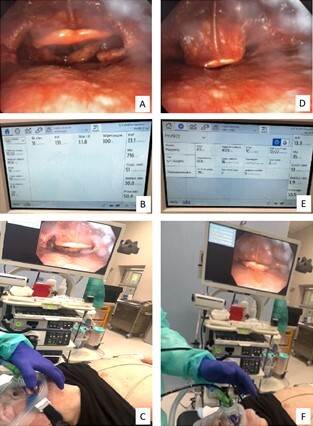
Presentation of cases:
Five patients requiring different bronchoscopy procedures were included in this retrospective case series. Two of them suffered from airway obstruction caused by laryngeal tumors, one from foreign body aspiration complicated with recurrent pneumonia, one from ventilator-associated pneumonia and one from RF in the course of ischemic stroke. FOB was safely performed in every patient despite the presence of relative contraindications in each case. Due to respiratory distress, FOB was supported with HFNC or NIV based on the patient’s overall condition and pathomechanism of RF. The parameters of HFNC and NIV were set according to ongoing randomized controlled trials.
Conclusions:
Active oxygen therapies, like HFNC and NIV, are promising methods of management in pa-tients with a high risk of RF during FOB.
Fiberoptic bronchoscopy (FOB) is a minimally invasive procedure which improves diagnostics and therapeutic management in patients with lung-related conditions. Although it is a generally well-tolerated intervention and there are only few contraindications for FOB, it has to be acknowledged that it causes acute narrowing of the airways and patients with inadequate oxygenation and respiratory acidosis may be disqualified from bronchoscopy due to an increased risk of respiratory failure (RF) development. Noninvasive techniques such as a high-flow nasal cannula (HFNC) and non-invasive ventilation (NIV) are accepted methods of respiratory support in patients with RF, however, their usage in patients undergoing FOB is still poorly represented in the literature.
Presentation of cases:
Five patients requiring different bronchoscopy procedures were included in this retrospective case series. Two of them suffered from airway obstruction caused by laryngeal tumors, one from foreign body aspiration complicated with recurrent pneumonia, one from ventilator-associated pneumonia and one from RF in the course of ischemic stroke. FOB was safely performed in every patient despite the presence of relative contraindications in each case. Due to respiratory distress, FOB was supported with HFNC or NIV based on the patient’s overall condition and pathomechanism of RF. The parameters of HFNC and NIV were set according to ongoing randomized controlled trials.
Conclusions:
Active oxygen therapies, like HFNC and NIV, are promising methods of management in pa-tients with a high risk of RF during FOB.
REFERENCES (21)
1.
Oraczewska A., Cofta S., Warcholiński A., Trejnowska E., Brożek G., Swinarew A. et al. The use of non-invasive respiratory assistance to facilitate bronchofiberoscopy performance in patients with hypoxemic (type one) respiratory failure – Study protocol. Adv. Med. Sci. 2023; 68(2): 474–481, doi: 10.1016/j.advms.2023.10.011.
2.
Danel A., Tobiczyk E., Warcholiński A., Trzaska-Sobczak M., Swinarew A., Brożek G. et al. May noninvasive mechanical ventilation and/ or continuous positive airway pressure increase the bronchoalveolar lavage salvage in patients with pulmonary diseases? Randomized clinical trial – Study protocol. Adv. Med. Sci. 2023; 68(2): 482–490, doi: 10.1016/j.advms.2023.10.009.
3.
Skoczyński S., Minarowski Ł., Tobiczyk E., Oraczewska A., Glinka K.., Ficek K. et al. Noninvasive ventilation-facilitated bronchofiberoscopy in patients with respiratory failure. Adv. Exp. Med. Biol. 2019; 1160: 53–64, doi: 10.1007/5584_2019_375.
4.
Skoczyński S., Ogonowski M., Tobiczyk E., Krzyżak D., Brożek G., Wierzbicka A. et al. Risk factors of complications during noninvasive mechanical ventilation -assisted flexible bronchoscopy. Adv. Med. Sci. 2021; 66(2): 246–253, doi: 10.1016/j.advms.2021.04.001.
5.
Skoczynski S., Wyskida K., Rzepka-Wrona P., Wyskida M., Uszok-Gawel E., Bartocha D. et al. Novel method of noninvasive ventilation supported therapeutic lavage in pulmonary alveolar proteinosis proves to relieve dyspnea, normalize pulmonary function test results and recover exercise capacity: a short communication. J. Thorac. Dis. 2018; 10(4): 2467–2473, doi: 10.21037/jtd.2018.04.12.
6.
Yilmazel Ucar E., Araz Ö., Kerget B., Akgun M., Saglam L. Comparison of high-flow and conventional nasal cannula oxygen in patients undergoing endobronchial ultrasonography. Intern. Med. J. 2021; 51(11): 1935–1939, doi: 10.1111/imj.15001.
7.
Du Rand I.A., Blaikley J., Booton R., Chaudhuri N., Gupta V., Khalid S. et al. British Thoracic Society guideline for diagnostic flexible bronchosco-py in adults: accredited by NICE. Thorax 2013; 68 Supp 1: i1–i44, doi: 10.1136/thoraxjnl-2013-203618.
8.
Roca O., Messika J., Caralt B., García-de-Acilu M., Sztrymf B., Ricard J.D. et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. J. Crit. Care 2016; 35: 200–205, doi: 10.1016/j.jcrc.2016.05.022.
9.
Pelaia C., Bruni A., Garofalo E., Rovida S., Arrighi E., Cammarota G. et al. Oxygenation strategies during flexible bronchoscopy: a review of the literature. Respir. Res. 2021; 22(1): 253, doi: 10.1186/s12931-021-01846-1.
10.
Sharma S., Danckers M., Sanghavi D.K., Chakraborty R.K. High-Flow Nasal Cannula. [Updated 2023 Apr 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/b... [accessed on 25 May 2024].
11.
Rochwerg B., Brochard L., Elliott M.W., Hess D., Hill N.S., Nava S. et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur. Respir. J. 2017; 50(2): 1602426, doi: 10.1183/13993003.02426-2016.
12.
Su C.L., Chiang L.L., Tam K.W., Chen T.T., Hu M.C. High-flow nasal cannula for reducing hypoxemic events in patients undergoing bronchoscopy: A systematic review and meta-analysis of randomized trials. PLoS One 2021; 16(12): e0260716, doi: 10.1371/journal.pone.0260716.
13.
Thiruvenkatarajan V., Sekhar V., Wong D.T., Currie J., Van Wijk R., Ludbrook G.L. Effect of high-flow nasal oxygen on hypoxaemia during procedural sedation: a systematic review and meta-analysis. Anaesthesia 2023; 78(1): 81–92, doi: 10.1111/anae.15845.
14.
Corral-Blanco M., Sayas-Catalán J., Hernández-Voth A., Rey-Terrón L., Villena-Garrido V. High-flow nasal cannula therapy as an adjuvant therapy for respiratory support during endoscopic techniques: A narrative review. J. Clin. Med. 2023; 13(1): 81, doi: 10.3390/jcm13010081.
15.
De Jong A., Chanques G., Jaber S. Mechanical ventilation in obese ICU patients: from intubation to extubation. Crit. Care 2017; 21(1): 63, doi: 10.1186/s13054-017-1641-1.
16.
Esquinas A., Zuil M., Scala R., Chiner E. Bronchoscopy during non-invasive mechanical ventilation: a review of techniques and procedures. Arch. Bronconeumol. 2013; 49(3): 105–112, doi: 10.1016/j.arbres.2012.05.008.
17.
Papazian L., Klompas M., Luyt C.E. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020; 46(5): 888–906, doi: 10.1007/s00134-020-05980-0.
18.
Campbell M., Sapra A. Physiology, Airflow Resistance. 2023 Apr 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 32119288.
19.
Mora Carpio A.L., Mora J.I. Positive End-Expiratory Pressure. 2023 Aug 14. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 28722933.
20.
Miller R.J., Casal R.F., Lazarus D.R., Ost D.E., Eapen G.A. Flexible bronchoscopy. Clin. Chest Med. 2018; 39(1): 1–16, doi: 10.1016/j.ccm.2017.09.002.
21.
Sircar M., Jha O.K., Chabbra G.S., Bhattacharya S. Noninvasive ventilation-assisted bronchoscopy in high-risk hypoxemic patients. Indian J. Crit. Care Med. 2019; 23(8): 363–367, doi: 10.5005/jp-journals-10071-23219.
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.