Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
The incidence of balanitis xerotica obliterans in patients surgically treated for phimosis
1
Department of Children’s Developmental Defects Surgery and Traumatology, Faculty of Medical Sciences in Zabrze,
Medical University of Silesia, Katowice, Poland
Corresponding author
Paweł Pobudejski
Klinika Chirurgii Wad Rozwojowych Dzieci i Traumatologii, SPSK Nr 1 im. prof. S. Szyszko ŚUM, ul. 3 Maja 13, 41-800 Zabrze
Klinika Chirurgii Wad Rozwojowych Dzieci i Traumatologii, SPSK Nr 1 im. prof. S. Szyszko ŚUM, ul. 3 Maja 13, 41-800 Zabrze
Ann. Acad. Med. Siles. 2024;78:330-335
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Phimosis is a disease entity that society has given negative connotations. Discussions about the foreskin, both in the context of its pathological and physiological conditions have been going on for centuries, and include issues related to religion, hygiene, esthetics and tradition. In 2002, researchers from London recognised that secondary phimosis corresponds to lichen sclerosus et atrophicus, better known as balanitis xerotica obliterans (BXO), constituting it the only absolute indication for circumcision in boys. This study aims to assess the histopathological examinations of patients after the surgical treatment of phimosis in order to ascertain the relationship between BXO and clinically diagnosed phimosis.
Material and methods:
This study analyzed the results of histopathological examinations in patients who underwent surgical methods of phimosis treatment in the period from January 2014 to March 2020. The inclusion criteria of the study were the surgical treatment of phimosis with the accompanying histopathological examination of the specimens collected during the surgery. The data were collected prospectively and randomly.
Results:
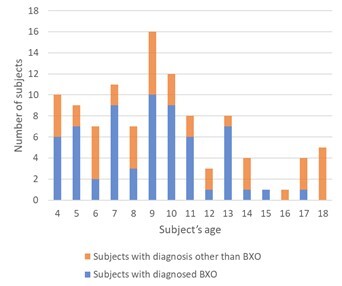
There were 106 patients in whom a surgical procedure and histopathological examination were performed. The mean age of the patients was 9.41 ± 3.82 years. In the entire group of patients, the diagnosis of BXO (including BXO focal) was 59% (n = 63).
Conclusions:
The most common cause of secondary phimosis after surgical treatment is BXO, with a patient prevalence ranging from 5.5% to 84%. The results of this study fall within this range. Visible scarring of the foreskin may also be caused by other factors such as chronic inflammation of the foreskin, but also poor hygiene or infections in this area.
Phimosis is a disease entity that society has given negative connotations. Discussions about the foreskin, both in the context of its pathological and physiological conditions have been going on for centuries, and include issues related to religion, hygiene, esthetics and tradition. In 2002, researchers from London recognised that secondary phimosis corresponds to lichen sclerosus et atrophicus, better known as balanitis xerotica obliterans (BXO), constituting it the only absolute indication for circumcision in boys. This study aims to assess the histopathological examinations of patients after the surgical treatment of phimosis in order to ascertain the relationship between BXO and clinically diagnosed phimosis.
Material and methods:
This study analyzed the results of histopathological examinations in patients who underwent surgical methods of phimosis treatment in the period from January 2014 to March 2020. The inclusion criteria of the study were the surgical treatment of phimosis with the accompanying histopathological examination of the specimens collected during the surgery. The data were collected prospectively and randomly.
Results:
There were 106 patients in whom a surgical procedure and histopathological examination were performed. The mean age of the patients was 9.41 ± 3.82 years. In the entire group of patients, the diagnosis of BXO (including BXO focal) was 59% (n = 63).
Conclusions:
The most common cause of secondary phimosis after surgical treatment is BXO, with a patient prevalence ranging from 5.5% to 84%. The results of this study fall within this range. Visible scarring of the foreskin may also be caused by other factors such as chronic inflammation of the foreskin, but also poor hygiene or infections in this area.
FUNDING
The work was not sponsored or funded by any external source or institution.
CONFLICT OF INTEREST
The authors have no competing interests to declare.
REFERENCES (17)
1.
Essentials of Paediatric Urology. D.F.M. Thomas, P.G. Duffy, A.M.K. Rickwood [ed.]. 2nd ed. Boca Raton: CRC Press, 2008.
2.
Principles and Practice of Surgery. O.J. Garden, A.W. Bradbury, J.L.R. Forsythe, R.W. Parks [ed.]. 6th ed. Elsevier, 2012.
3.
EAU Guidelines. Edn. presented at the EAU Annual Congress Milan 2021. ISBN 978-94-92671-13-4.
4.
Oster J. Further fate of the foreskin. Incidence of preputial adhesions, phimosis, and smegma among Danish schoolboys. Arch. Dis. Child. 1968; 43(228): 200–203, doi: 10.1136/adc.43.228.200.
5.
Charlton O.A., Smith S.D. Balanitis xerotica obliterans: a review of diagnosis and management. Int. J. Dermatol. 2019; 58(7): 777–781, doi: 10.1111/ijd.14236.
6.
Kiss A., Király L., Kutasy B., Merksz M. High incidence of balanitis xerotica obliterans in boys with phimosis: prospective 10-year study. Pediatr. Dermatol. 2005; 22(4): 305–308, doi: 10.1111/j.1525-1470.2005.22404.x.
7.
Meffert J.J., Davis B.M., Grimwood R.E. Lichen sclerosus. J. Am. Acad. Dermatol. 1995; 32(3): 393–418, doi: 10.1016/0190-9622(95)90060-8.
8.
Meyer M., Müller A.K., Yang J., Ŝulcová J., Werner S. The role of chronic inflammation in cutaneous fibrosis: fibroblast growth factor recep-tor deficiency in keratinocytes as an example. J. Investig. Dermatol. Symp. Proc. 2011; 15(1): 48–52, doi: 10.1038/jidsymp.2011.1.
9.
Morris B.J., Krieger J.N. Penile inflammatory skin disorders and the preventive role of circumcision. Int. J. Prev. Med. 2017; 8: 32, doi: 10.4103/ijpvm.IJPVM_377_16.
10.
Kikiros C., Beasley S., Woodward A.A. The response of phimosis to local steroid application. Pediatr. Surg. Int. 1993; 8(4): 329–332, doi: 10.1007/bf00173357.
11.
Ghidini F., Virgone C., Pulvirenti R., Trovalusci E., Gamba P. Could a careful clinical examination distinguish physiologic phimosis from balanitis xerotica obliterans in children? Eur. J. Pediatr. 2021; 180(2): 591–595, doi: 10.1007/s00431-020-03881-4.
12.
Jayakumar S., Antao B., Bevington O., Furness P., Ninan G.K. Balanitis xerotica obliterans in children and its incidence under the age of 5 years. J. Pediatr. Urol. 2012; 8(3): 272–275, doi: 10.1016/j.jpurol.2011.05.001.
13.
Celis S., Reed F., Murphy F., Adams S., Gillick J., Abdelhafeez A.H. et al. Balanitis xerotica obliterans in children and adolescents: A literature review and clinical series. J. Pediatr. Urol. 2014; 10(1): 34–39, doi: 10.1016/j.jpurol.2013.09.027.
14.
Boksh K., Patwardhan N. Balanitis xerotica obliterans: has its diagnostic accuracy improved with time? JRSM Open 2017; 8(6): 2054270417692731, doi: 10.1177/2054270417692731.
15.
Bochove-Overgaauw D.M., Gelders W., De Vylder A.M. Routine biopsies in pediatric circumcision: (non) sense? J. Pediatr. Urol. 2009; 5(3): 178–180, doi: 10.1016/j.jpurol.2008.11.008.
16.
Yardley I.E., Cosgrove C., Lambert A.W. Paediatric preputial pathology: are we circumcising enough? Ann. R. Coll. Surg. Engl. 2007; 89(1): 62–65, doi: 10.1308/003588407X160828.
17.
Shankar K.R., Rickwood A.M. The incidence of phimosis in boys. BJU Int. 1999; 84(1): 101–102, doi: 10.1046/j.1464-410x.1999.00147.x.
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.