Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
The Virtual Clinic application – a new solution for modern medical education
1
Department of Radiology and Nuclear Medicine, Medical University of Silesia, Katowice, Poland
2
Department of Neurology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
3
Department of Internal Medicine, Autoimmune and Metabolic Diseases, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
4
National Research Institute of Oncology, Gliwice, Poland
5
Department of Physiology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
6
BD Polska, Warsaw, Poland
7
Department of Medical Informatics and Telemedicine, Medical University of Warsaw, Poland
8
Department of Biochemistry, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
Corresponding author
Mateusz Winder
Department of Radiology and Nuclear Medicine, Medical University of Silesia, Katowice, Poland
Department of Radiology and Nuclear Medicine, Medical University of Silesia, Katowice, Poland
Ann. Acad. Med. Siles. 2024;78:287-293
KEYWORDS
TOPICS
ABSTRACT
Introduction:
The abrupt transition to remote learning caused by the COVID-19 pandemic clearly indicated the need to implement radical technological and institutional changes to the current approach to teaching. Virtual reality (VR) and artificial intelligence (AI) assisted programs have emerged as the new and effective methods utilized in education and medical training.
Material and methods:
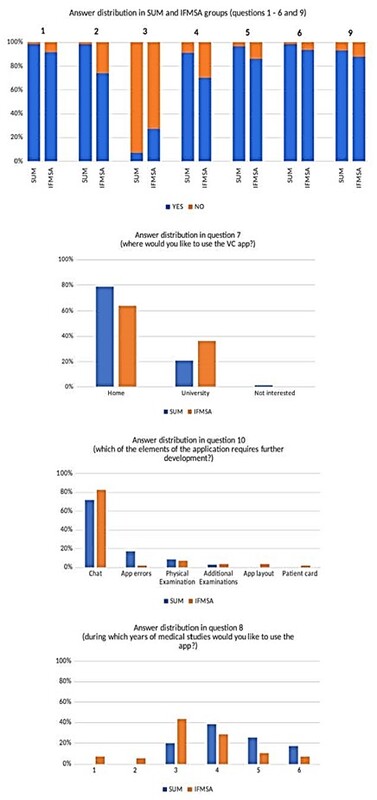
The Virtual Clinic (VC) is a new online application developed by Polish medical universities which implement AI algorithms to teach students the medical interview including obtaining patients medical history, performing a physical examination as well as diagnostics and treatment planning. Our study enrolled 164 medical students who tested the VC and completed an online questionnaire.
Results:
The results of the survey showed that 93.9% of the respondents believe that the VC will prove effective as an educational tool supporting teaching at faculties of medicine and health sciences.
Conclusions:
Our preliminary experiences suggest that the use of AI assisted programs such as the VC seems highly anticipated and justified in medical higher education.
The abrupt transition to remote learning caused by the COVID-19 pandemic clearly indicated the need to implement radical technological and institutional changes to the current approach to teaching. Virtual reality (VR) and artificial intelligence (AI) assisted programs have emerged as the new and effective methods utilized in education and medical training.
Material and methods:
The Virtual Clinic (VC) is a new online application developed by Polish medical universities which implement AI algorithms to teach students the medical interview including obtaining patients medical history, performing a physical examination as well as diagnostics and treatment planning. Our study enrolled 164 medical students who tested the VC and completed an online questionnaire.
Results:
The results of the survey showed that 93.9% of the respondents believe that the VC will prove effective as an educational tool supporting teaching at faculties of medicine and health sciences.
Conclusions:
Our preliminary experiences suggest that the use of AI assisted programs such as the VC seems highly anticipated and justified in medical higher education.
FUNDING
This research was supported by the National Centre for Research and Development - NCBR (POIR.01.01.01-00-0526/19).
CONFLICT OF INTEREST
None declared.
REFERENCES (18)
1.
Rajab M.H., Gazal A.M., Alkattan K. Challenges to online medical education during the COVID-19 pandemic. Cureus 2020; 12(7): e8966, doi: 10.7759/cureus.8966.
2.
Lee J., Wu A.S., Li D., Kulasegaram K.M. Artificial intelligence in undergraduate medical education: A scoping review. Acad. Med. 2021; 96(11S): S62–S70, doi: 10.1097/ACM.0000000000004291.
3.
Curtis M.T., DiazGranados D., Feldman M. Judicious use of simulation technology in continuing medical education. J. Contin. Educ. Health Prof. 2012; 32(4): 255–260, doi: 10.1002/chp.21153.
4.
Okuda Y., Bryson E.O., DeMaria S. Jr, Jacobson L., Quinones J., Shen B. et al. The utility of simulation in medical education: what is the evidence? Mt. Sinai J. Med. 2009; 76(4): 330–343, doi: 10.1002/msj.20127.
5.
Chakravarthy B., Ter Haar E., Bhat S.S., McCoy C.E., Denmark T.K., Lotfipour S. Simulation in medical school education: review for emergency medicine. West. J. Emerg. Med. 2011; 12(4): 461–466, doi: 10.5811/westjem.2010.10.1909.
6.
UNESCO. Beijing Consensus on Artificial Intelligence and Education. Unesco / UNESDOC Digital Library, 2019 [online] https://unesdoc.unesco.org/ark... [accessed on 14 April 2023].
7.
Carin L. On artificial intelligence and deep learning within medical education. Acad. Med. 2020; 95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations): S10–S11, doi: 10.1097/ACM.0000000000003630.
8.
Mahmood T., Scaffidi M.A., Khan R., Grover S.C. Virtual reality simulation in endoscopy training: Current evidence and future directions. World J. Gastroenterol. 2018; 24(48): 5439–5445, doi: 10.3748/wjg.v24.i48.5439.
9.
United Nations. Policy Brief: Education during COVID-19 and beyond, 2020 [online] https://www.un.org/development... [accessed on 22 May 2023].
10.
Naciri A., Radid M., Kharbach A., Chemsi G. E-learning in health professions education during the COVID-19 pandemic: a systematic review. J. Educ. Eval. Health Prof. 2021; 18: 27, doi: 10.3352/jeehp.2021.18.27.
11.
Bączek M., Zagańczyk-Bączek M., Szpringer M., Jaroszyński A., Wożakowska-Kapłon B. Students’ perception of online learning during the COVID-19 pandemic: A survey study of Polish medical students. Medicine (Baltimore) 2021; 100(7): e24821, doi: 10.1097/MD.0000000000024821.
12.
O’Doherty D., Dromey M., Lougheed J., Hannigan A., Last J., McGrath D. Barriers and solutions to online learning in medical education – an integrative review. BMC Med. Educ. 2018; 18(1): 130, doi: 10.1186/s12909-018-1240-0.
13.
Elessawy M., Mabrouk M., Heilmann T., Weigel M., Zidan M., Abu-Sheasha G. et al. Evaluation of laparoscopy virtual reality training on the improvement of trainees’ surgical skills. Medicina (Kaunas) 2021; 57(2): 130, doi: 10.3390/medicina57020130.
14.
Paluch A., Lakpriya S., Moyes S., Evans L. From laptop to laparotomy: A retrospective evaluation of virtual teaching methods in surgical anatomy during COVID-19. Br. J. Surg. 2021; 108(Suppl 6): znab259.861, doi: 10.1093/bjs/znab259.861.
15.
Siau K., Hodson J., Neville P., Turner J., Beale A., Green S. et al. Impact of a simulation-based induction programme in gastroscopy on trainee outcomes and learning curves. World J. Gastrointest. Endosc. 2020; 12(3): 98–110, doi: 10.4253/wjge.v12.i3.98.
16.
Qiao W., Bai Y., Lv R., Zhang W., Chen Y., Lei S. et al. The effect of virtual endoscopy simulator training on novices: a systematic review. PLoS One 2014; 9(2): e89224, doi: 10.1371/journal.pone.0089224.
17.
Al-Elq A.H. Simulation-based medical teaching and learning. J. Family Community Med. 2010; 17(1): 35–40, doi: 10.4103/1319-1683.68787.
18.
Kalaniti K., Campbell D.M. Simulation-based medical education: time for a pedagogical shift. Indian Pediatr. 2015; 52(1): 41–45, doi: 10.1007/s13312-015-0565-6.
Share
RELATED ARTICLE
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.