Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
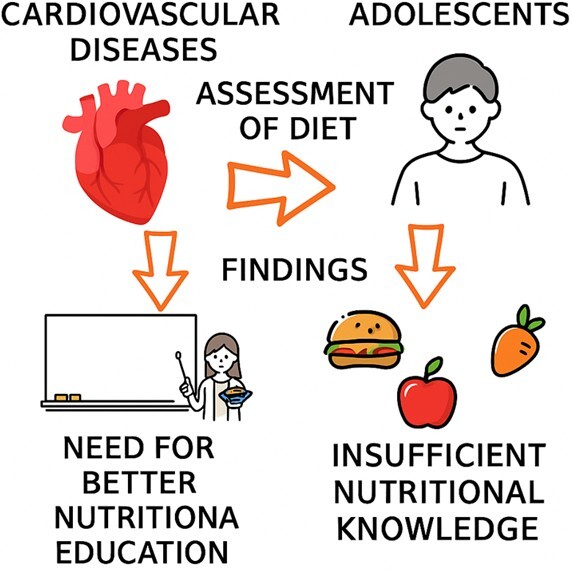
Dietary patterns and cardiovascular risk in adolescent males: An epidemiological study among high school students in Silesia, Poland
1
Students’ Scientific Club, Department of Public Health, Faculty of Public Health in Bytom, Medical University of Silesia, Katowice, Poland
2
Department of Epidemiology, Faculty of Public Health in Bytom, Medical University of Silesia, Katowice, Poland
3
Department of Economics and Health Care Management, Faculty of Public Health in Bytom,
Medical University of Silesia, Katowice, Poland
4
Students’ Scientific Club, Department of Epidemiology, Faculty of Public Health in Bytom, Medical University of Silesia, Katowice, Poland
5
Department of Public Health, Faculty of Public Health in Bytom, Medical University of Silesia, Katowice, Poland
Corresponding author
Martyna Szymańska
Studenckie Koło Naukowe, Zakład Zdrowia Publicznego, Wydział Zdrowia Publicznego w Bytomiu ŚUM, ul. Piekarska 18, 41-902 Bytom
Studenckie Koło Naukowe, Zakład Zdrowia Publicznego, Wydział Zdrowia Publicznego w Bytomiu ŚUM, ul. Piekarska 18, 41-902 Bytom
Ann. Acad. Med. Siles. 2025;79:288-295
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Cardiovascular diseases (CVDs) are a major cause of mortality globally, including in Poland. Their risk factors include both non-modifiable (e.g., age or genetics) and modifiable elements (e.g., diet and physical activity). Among the latter, diet plays a pivotal role in prevention. Poor dietary habits – such as high intake of saturated fats and low consumption of fruits and vegetables – significantly increase CVDs risk. The aim of this study was to assess the risk of developing CVDs among adolescents based on their dietary habits.
Material and methods:
The research, conducted in May 2024, involved 583 male students from School No. 10 in Zabrze, Poland. An anonymous questionnaire gathered information on eating habits, meal composition, food preparation, and seasoning practices. Statistical analysis was carried out using Microsoft Excel, including chi-square tests and correlation analysis.
Results:
Results showed that 78.8% of participants had a normal BMI, 14.1% were overweight, and 2% were obese. About 50% rated their nutritional knowledge as good. A moderate positive correlation was found between nutritional knowledge and physical activity (r = 0.34; p < 0.05). While daily vegetable consumption was 54%, fruit consumption was slightly lower, at 48%. A high intake of saturated fats and insufficient consumption of fruits and vegetables were significantly linked to increased CVDs risk (χ² = 34.36; p < 0.0001).
Conclusions:
Despite normal BMI values among participants, the findings highlight the need to strengthen nutrition education. The unbalanced dietary pattern and excessive intake of saturated fats justify implementing preventive measures aimed at reducing cardiovascular risk and promoting healthier habits in adolescents.
Cardiovascular diseases (CVDs) are a major cause of mortality globally, including in Poland. Their risk factors include both non-modifiable (e.g., age or genetics) and modifiable elements (e.g., diet and physical activity). Among the latter, diet plays a pivotal role in prevention. Poor dietary habits – such as high intake of saturated fats and low consumption of fruits and vegetables – significantly increase CVDs risk. The aim of this study was to assess the risk of developing CVDs among adolescents based on their dietary habits.
Material and methods:
The research, conducted in May 2024, involved 583 male students from School No. 10 in Zabrze, Poland. An anonymous questionnaire gathered information on eating habits, meal composition, food preparation, and seasoning practices. Statistical analysis was carried out using Microsoft Excel, including chi-square tests and correlation analysis.
Results:
Results showed that 78.8% of participants had a normal BMI, 14.1% were overweight, and 2% were obese. About 50% rated their nutritional knowledge as good. A moderate positive correlation was found between nutritional knowledge and physical activity (r = 0.34; p < 0.05). While daily vegetable consumption was 54%, fruit consumption was slightly lower, at 48%. A high intake of saturated fats and insufficient consumption of fruits and vegetables were significantly linked to increased CVDs risk (χ² = 34.36; p < 0.0001).
Conclusions:
Despite normal BMI values among participants, the findings highlight the need to strengthen nutrition education. The unbalanced dietary pattern and excessive intake of saturated fats justify implementing preventive measures aimed at reducing cardiovascular risk and promoting healthier habits in adolescents.
REFERENCES (46)
1.
Thiriet M. Cardiovascular disease: An introduction. In: Vasculopathies. Biomathematical and Biomechanical Modeling of the Circulatory and Ventilatory Systems. Vol 8. Springer. Cham 2019, p. 1–90, doi: 10.1007/978-3-319-89315-0_1.
2.
Cardiovascular diseases (CVDs). WHO, 2021 [online] https://www.who.int/news-room/...) [accessed on 11 April 2025].
3.
Gózd-Barszczewska A.I., Panasiuk L. Prevalence of modifiable cardiovascular risk factors in patients hospitalized due to symptomatic coronary artery disease in the Lublin Province. [Article in Polish]. Med. Og. Nauk. Zdr. 2021; 27(4): 453–560, doi: 10.26444/monz/144082.
4.
Pahwa R., Jialal I. Atherosclerosis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023, https://www.ncbi.nlm.nih.gov/b... [accessed on 11 April 2025].
5.
Shahjehan R.D., Sharma S., Bhutta B.S. Coronary artery disease. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023, https://www.ncbi.nlm.nih.gov/b... [accessed on 11 April 2025].
6.
Khaku A.S., Tadi P. Cerebrovascular disease. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023, https://www.ncbi.nlm.nih.gov/b... [accessed on 11 April 2025].
7.
About peripheral arterial disease (PAD). CDC, May 15, 2024 [online] https://www.cdc.gov/heart-dise... [accessed on 11 April 2025].
8.
Global atlas on cardiovascular disease prevention and control. WHO, 12 May 2011 [online] https://www.who.int/publicatio... [accessed on 11 April 2025].
9.
Umieralność w 2021 roku. Zgony według przyczyn - dane wstępne. Główny Urząd Statystyczny, 16.05.2022 [online] https://stat.gov.pl/obszary-te... [accessed on 11 April 2025].
10.
Timmis A., Townsend N., Gale C.P., Torbica A., Lettino M., Petersen S.E. et al. European Society of Cardiology: Cardiovascular Disease Statistics 2019. Eur. Heart J. 2020; 41(1): 12–85, doi: 10.1093/eurheartj/ehz859.
11.
STEPS Manual / Part 1: Introduction and roles / Section 1: Introduction. WHO, 2023 [online] https://www.who.int/teams/nonc... [accessed on 11 April 2025].
12.
Kopeć M. Zachowania zdrowotne młodych osób dorosłych w kontekście profilaktyki chorób układu sercowo-naczyniowego. [MA Thesis]. Uniwersytet Jagielloński w Krakowie 2023, https://ruj.uj.edu.pl/xmlui/ha....
13.
Surma S., Szyndler A., Narkiewicz K. Świadomość nadciśnienia tętniczego i innych czynników ryzyka chorób układu sercowo-naczyniowego w populacji osób dorosłych. Chor. Serca Naczyń 2018; 15(1): 14–22.
14.
Gao Z., Chen Z., Sun A., Deng X. Gender differences in cardiovascular disease. Med. Nov. Technol. Devices 2019; 4: 100025, doi: 10.1016/j.medntd.2019.100025.
15.
Di Giosia P., Passacquale G., Petrarca M., Giorgini P., Marra A.M., Ferro A. Gender differences in cardiovascular prophylaxis: Focus on antiplatelet treatment. Pharmacol. Res. 2017; 119: 36–47, doi: 10.1016/j.phrs.2017.01.025.
16.
Maas A.H., Appelman Y.E. Gender differences in coronary heart disease. Neth. Heart J. 2010; 18(12): 598–602, doi: 10.1007/s12471-010-0841-y.
17.
Rodgers J.L., Jones J., Bolleddu S.I., Vanthenapalli S., Rodgers L.E., Shah K. et al. Cardiovascular risks associated with gender and aging. J. Cardiovasc. Dev. Dis. 2019; 6(2): 19, doi: 10.3390/jcdd6020019.
18.
Steenman M., Lande G. Cardiac aging and heart disease in humans. Biophys. Rev. 2017; 9(2): 131–137, doi: 10.1007/s12551-017-0255-9.
19.
Vrablik M., Dlouha D., Todorovova V., Stefler D., Hubacek J.A. Genetics of cardiovascular disease: How far are we from personalized CVD risk prediction and management? Int. J. Mol. Sci. 2021; 22(8): 4182, doi: 10.3390/ijms22084182.
20.
Cybulska B. Rodzinna hipercholesterolemia – zalecenia dietetyczne. NCEZ, 28 stycznia 2020 [online] https://ncez.pzh.gov.pl/chorob... [accessed on 11 April 2025].
21.
Bays H.E., Taub P.R., Epstein E., Michos E.D., Ferraro R.A., Bailey A.L. et al. Ten things to know about ten cardiovascular disease risk factors. Am. J. Prev. Cardiol. 2021; 5: 100149, doi: 10.1016/j.ajpc.2021.100149.
22.
Pinckard K., Baskin K.K., Stanford K.I. Effects of exercise to improve cardiovascular health. Front. Cardiovasc. Med. 2019; 6: 69, doi: 10.3389/fcvm.2019.00069.
23.
Obesity and overweight. WHO, 2024 [online] https://www.who.int/news-room/... [accessed on 11 April 2025].
24.
Zhang Y., Liu J., Yao J., Ji G., Qian L., Wang J. et al. Obesity: pathophysiology and intervention. Nutrients 2014; 6(11): 5153–5183, doi: 10.3390/nu6115153.
25.
Schwartz M.W., Seeley R.J., Zeltser L.M., Drewnowski A., Ravussin E., Redman L.M. et al. Obesity pathogenesis: An Endocrine Society Scientific Statement. Endocr. Rev. 2017; 38(4): 267–296, doi: 10.1210/er.2017-00111.
26.
Filippou C.D., Tsioufis C.P., Thomopoulos C.G., Mihas C.C., Dimitriadis K.S., Sotiropoulou L.I. et al. Dietary Approaches to Stop Hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: A systematic review and meta-analysis of randomized controlled trials. Adv. Nutr. 2020; 11(5): 1150–1160, doi: 10.1093/advances/nmaa041.
27.
Ravera A., Carubelli V., Sciatti E., Bonadei I., Gorga E., Cani D. et al. Nutrition and cardiovascular disease: Finding the perfect recipe for cardiovascular health. Nutrients 2016; 8(6): 363, doi: 10.3390/nu8060363.
28.
Casas R., Castro-Barquero S., Estruch R., Sacanella E. Nutrition and cardiovascular health. Int. J. Mol. Sci. 2018; 19(12): 3988, doi: 10.3390/ijms19123988.
29.
Malikowska K., Grabańska-Martyńska K. History of the Mediterranean diet in prevention of diseases of cardiovascular system. [Article in Polish]. Acta Medicorum Polonorum 2016; 6(1): 41–49.
30.
Kubica A., Sinkiewicz W., Szymański P., Bogdan M. Edukacja zdrowotna w chorobach układu krążenia – możliwości i zagrożenia. Folia Cardiol. Excerpta 2006; 1(4): 177–188.
31.
Profilaktyka pierwotna. Portal Gov.pl, 2017 [online] https://www.gov.pl/web/zdrowie... [accessed on 11 April 2025].
32.
Sinai T., Axelrod R., Shimony T., Boaz M., Kaufman-Shriqui V. Dietary patterns among adolescents are associated with growth, socioeconomic features, and health-related behaviors. Foods 2021; 10(12): 3054, doi: 10.3390/foods10123054.
33.
Suman S., Pravalika J., Manjula P., Farooq U. Gender and CVD – does it really matters? Curr. Probl. Cardiol. 2023; 48(5): 101604, doi: 10.1016/j.cpcardiol.2023.101604.
34.
Willett W. Nutritional Epidemiology. 3rd ed. Oxford University Press. New York, NY 2013, doi: 10.1093/acprof:oso/9780199754038.001.0001.
35.
Cade J., Thompson R., Burley V., Warm D. Development, validation and utilisation of food-frequency questionnaires – a review. Public Health Nutr. 2002; 5(4): 567–587, doi: 10.1079/PHN2001318.
36.
Shields M., Gorber S.C., Tremblay M.S. Estimates of obesity based on self-report versus direct measures. Health Rep. 2008; 19(2): 61–76.
37.
Nutbeam D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000; 15(3): 259–267, doi: 10.1093/heapro/15.3.259.
38.
Spear B.A. Adolescent Growth and Development. In: J. Stang, M. Story [ed.]. Guidelines for Adolescent Nutrition Services. University of Minnesota: Minneapolis, MN, USA, 2005, p. 1–8.
39.
Piramida Zdrowego Żywienia i Aktywności Fizycznej dla dorosłych. M. Jarosz i in. [oprac.]. Instytut Żywności i Żywienia. Narodowe Centrum Edukacji Żywieniowej, 31.03.2021 [online] https://ncez.pzh.gov.pl/sdm_do... [accessed on 11 April 2025].
40.
He F.J., Nowson C.A., MacGregor G.A. Fruit and vegetable consumption and stroke: meta-analysis of cohort studies. Lancet 2006; 367(9507): 320–326, doi: 10.1016/S0140-6736(06)68069-0.
41.
European Food Safety Authority (EFSA). Scientific Opinion on the safety of caffeine. EFSA J. 2015; 13(5): 4102, doi: 10.2903/j.efsa.2015.4102.
42.
Seifert S.M., Schaechter J.L., Hershorin E.R., Lipshultz S.E. Health effects of energy drinks on children, adolescents, and young adults. Pediatrics 2011; 127(3): 511–528, doi: 10.1542/peds.2009-3592.
43.
Schwingshackl L., Hoffmann G. Monounsaturated fatty acids, olive oil and health status: a systematic review and meta-analysis of cohort studies. Lipids Health Dis. 2014; 13: 154, doi: 10.1186/1476-511X-13-154.F.
44.
Sodium reduction. WHO, 7 February 2025 [online] https://www.who.int/news-room/... [accessed on 11 April 2025].
45.
Malczyk E. Nutritional status of children and youth in Poland on basis of literature from last ten years (2005–2015). [Article in Polish]. Ann. Acad. Med. Siles. 2016; 70: 56–65, doi: 10.18794/aams/58971.
46.
Lissner L., Troiano R.P., Midthune D., Heitmann B.L., Kipnis V., Subar A.F. et al. OPEN about obesity: recovery biomarkers, dietary reporting errors and BMI. Int. J. Obes. 2007; 31(6): 956–961, doi: 10.1038/sj.ijo.0803527.
Share
RELATED ARTICLE
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.