Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Does the COVID-19 pandemic have an impact on fears and concerns among pregnant women?
1
Students’ Scientific Club, Department of Gynaecology and Obstetrics, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
2
Department of Gynaecology and Obstetrics, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
Corresponding author
Mateusz Zabochnicki
Katedra i Klinika Ginekologii i Położnictwa, Śląski Uniwersytet Medyczny w Katowicach, ul. Medyków 14, 40-752 Katowice
Katedra i Klinika Ginekologii i Położnictwa, Śląski Uniwersytet Medyczny w Katowicach, ul. Medyków 14, 40-752 Katowice
Ann. Acad. Med. Siles. 2024;78:309-316
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Anxiety and depressive symptoms are common during pregnancy. The occurrence of the COVID-19 virus pandemic is a unique stressor that affected the psychological course of delivery. The aim of the work is to evaluate the impact of the COVID-19 pandemic on the course of pregnancy and childbirth among the Polish population.
Material and methods:
The study group consisted of 2186 women. A questionnaire survey was conducted between November 2020 and December 2020 via the Internet. The inclusion criterion was pregnancy and childbirth during the COVID-19 pandemic. The authors’ questions, with a five-point Likert scale, were used to assess concern and discomfort.
Results:
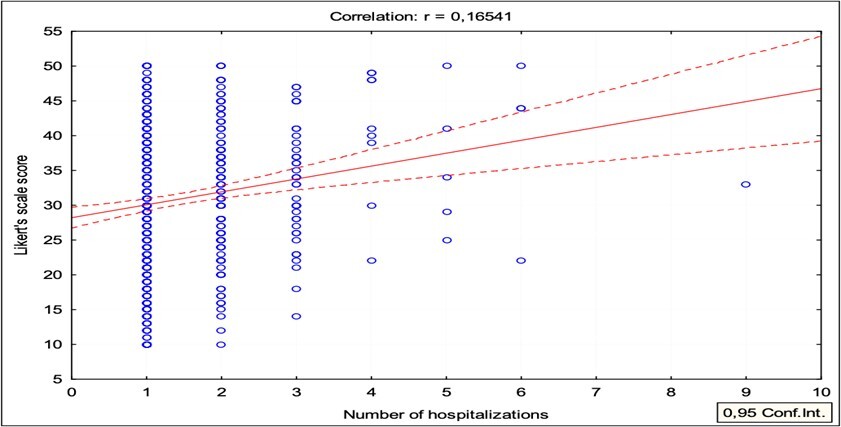
Women hospitalized during pregnancy had more pregnancy-related fears and concerns (mean 30.9 vs 29.6; p = 0.007). A similar relationship was found for women who had a cesarean section (30.6 vs 29.5; p = 0.006) or were hospitalized > 7 days (31.8 vs 29.7; p = 0.012). A statistically significant weak correlation was found between the mean scores of the concern questions and the number of hospitalizations during pregnancy (Pearson correlation coefficient r = 0.1654; p < 0.000).
Conclusions:
This study found alarmingly high levels of anxiety in pregnant women during the COVID-19 pandemic, which may have long-term implications for their children.
Anxiety and depressive symptoms are common during pregnancy. The occurrence of the COVID-19 virus pandemic is a unique stressor that affected the psychological course of delivery. The aim of the work is to evaluate the impact of the COVID-19 pandemic on the course of pregnancy and childbirth among the Polish population.
Material and methods:
The study group consisted of 2186 women. A questionnaire survey was conducted between November 2020 and December 2020 via the Internet. The inclusion criterion was pregnancy and childbirth during the COVID-19 pandemic. The authors’ questions, with a five-point Likert scale, were used to assess concern and discomfort.
Results:
Women hospitalized during pregnancy had more pregnancy-related fears and concerns (mean 30.9 vs 29.6; p = 0.007). A similar relationship was found for women who had a cesarean section (30.6 vs 29.5; p = 0.006) or were hospitalized > 7 days (31.8 vs 29.7; p = 0.012). A statistically significant weak correlation was found between the mean scores of the concern questions and the number of hospitalizations during pregnancy (Pearson correlation coefficient r = 0.1654; p < 0.000).
Conclusions:
This study found alarmingly high levels of anxiety in pregnant women during the COVID-19 pandemic, which may have long-term implications for their children.
FUNDING
Not applicable.
CONFLICT OF INTEREST
Authors declare no conflict of interest.
REFERENCES (55)
1.
WHO Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020. World Health Organization, 11 March 2020 [online] https://www.who.int/dg/speeche... [accessed on 30 April 2022].
2.
Makowska M., Boguszewski R., Nowakowski M., Podkowińska M. Self-medication-related behaviors and Poland’s COVID-19 lockdown. Int. J. Environ. Res. Public Health 2020; 17(22): 8344, doi: 10.3390/ijerph17228344.
3.
Jones E.A.K., Mitra A.K., Bhuiyan A.R. Impact of COVID-19 on mental health in adolescents: A systematic review. Int. J. Environ. Res. Public Health 2021; 18(5): 2470, doi: 10.3390/ijerph18052470.
4.
Hossain M.M., Tasnim S., Sultana A., Faizah F., Mazumder H., Zou L. et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020; 9: 636, doi: 10.12688/f1000research.24457.1.
5.
Cohen S.D., Cukor D., Kimmel P.L. Anxiety in patients treated with hemodialysis. Clin. J. Am. Soc. Nephrol. 2016; 11(12): 2250–2255, doi: 10.2215/CJN.02590316.
6.
Miralles O., Sanchez-Rodriguez D., Marco E., Annweiler C., Baztan A., Betancor É. et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: a report from six European countries. Eur. Geriatr. Med. 2021; 12(1): 193–204, doi: 10.1007/s41999-020-00415-x.
7.
Şahi̇n D., Tanaçan A., Webster S.N., Moraloğlu Tekin Ö. Pregnancy and COVID-19: prevention, vaccination, therapy, and beyond. Turk. J. Med. Sci. 2021; 51(SI-1): 3312–3326, doi: 10.3906/sag-2106-134.
8.
Kohlhepp L.M., Hollerich G., Vo L., Hofmann-Kiefer K., Rehm M., Louwen F. et al. Physiological changes during pregnancy. [Article in German]. Anaesthesist 2018; 67(5): 383–396, doi: 10.1007/s00101-018-0437-2.
9.
Bjelica A., Cetkovic N., Trninic-Pjevic A., Mladenovic-Segedi L. The phenomenon of pregnancy — a psychological view. Ginekol. Pol. 2018; 89(2): 102–106, doi: 10.5603/GP.a2018.0017.
10.
Salem D., Katranji F., Bakdash T. COVID‐19 infection in pregnant women: Review of maternal and fetal outcomes. Int. J. Gynaecol. Obstet. 2021; 152(3): 291–298, doi: 10.1002/ijgo.13533.
11.
Schwartz D.A. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: Maternal coronavirus infections and pregnancy outcomes. Arch. Pathol. Lab. Med. 2020; 144(7): 799–805, doi: 10.5858/arpa.2020-0901-SA.
12.
Dashraath P., Wong J.L.J., Lim M.X.K., Lim L.M., Li S., Biswas A. et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020; 222(6): 521–531, doi: 10.1016/j.ajog.2020.03.021.
13.
Webster Marketon J.I., Glaser R. Stress hormones and immune function. Cell. Immunol. 2008; 252(1–2): 16–26, doi: 10.1016/j.cellimm.2007.09.006.
14.
Wastnedge E.A.N., Reynolds R.M., van Boeckel S.R., Stock S.J., Denison F.C., Maybin J.A. et al. Pregnancy and COVID-19. Physiol. Rev. 2021; 101(1): 303–318, doi: 10.1152/physrev.00024.2020.
15.
Servante J., Swallow G., Thornton J.G., Myers B., Munireddy S., Malinowski A.K. et al. Haemostatic and thrombo-embolic complications in pregnant women with COVID-19: a systematic review and critical analysis. BMC Pregnancy Childbirth 2021; 21(1): 108, doi: 10.1186/s12884-021-03568-0.
16.
Adeyanju G.C., Engel E., Koch L., Ranzinger T., Shahid I.B.M., Head M.G. et al. Determinants of influenza vaccine hesitancy among pregnant women in Europe: a systematic review. Eur. J. Med. Res. 2021; 26(1): 116, doi: 10.1186/s40001-021-00584-w.
17.
Wang C.L., Liu Y.Y., Wu C.H., Wang C.Y., Wang C.H., Long C.Y. Impact of COVID-19 on pregnancy. Int. J. Med. Sci. 2021; 18(3): 763–767, doi: 10.7150/ijms.49923.
18.
Jamieson D.J., Rasmussen S.A. An update on COVID-19 and pregnancy. Am. J. Obstet. Gynecol. 2022; 226(2): 177–186, doi: 10.1016/j.ajog.2021.08.054.
19.
Mah B.L., Pringle K.G., Weatherall L., Keogh L., Schumacher T., Eades S. et al. Pregnancy stress, healthy pregnancy and birth outcomes – the need for early preventative approaches in pregnant Australian Indigenous women: a prospective longitudinal cohort study. J. Dev. Orig. Health Dis. 2019; 10(1): 31–38, doi: 10.1017/S204017441800079X.
20.
Bayrampour H., Ali E., McNeil D.A., Benzies K., MacQueen G., Tough S. Pregnancy-related anxiety: A concept analysis. Int. J. Nurs. Stud. 2016; 55: 115–130, doi: 10.1016/j.ijnurstu.2015.10.023.
21.
van den Bergh B.R.H., Dahnke R., Mennes M. Prenatal stress and the developing brain: Risks for neurodevelopmental disorders. Dev. Psychopathol. 2018; 30(3): 743–762, doi: 10.1017/S0954579418000342.
22.
Silva M.M.J., Nogueira D.A., Clapis M.J., Leite E.P.R.C. Anxiety in pregnancy: prevalence and associated factors. Rev. Esc. Enferm. USP. 2017; 51: e03253, doi: 10.1590/S1980-220X2016048003253.
23.
Biaggi A., Conroy S., Pawlby S., Pariante C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016; 191: 62–77, doi: 10.1016/j.jad.2015.11.014.
24.
Oliveira C., Imakawa T.D.S., Moisés E.C.D. Physical activity during pregnancy: Recommendations and assessment tools. Rev. Bras. Ginecol. Obstet. 2017; 39(8): 424–432, doi: 10.1055/s-0037-1604180.
25.
Thomas J.C., Letourneau N., Campbell T.S., Giesbrecht G.F. Social buffering of the maternal and infant HPA axes: Mediation and moderation in the intergenerational transmission of adverse childhood experiences. Dev. Psychopathol. 2018; 30(3): 921–939, doi: 10.1017/S0954579418000512.
26.
Naghizadeh S., Mirghafourvand M. Relationship of fear of COVID-19 and pregnancy-related quality of life during the COVID-19 pandemic. Arch. Psychiatr. Nurs. 2021; 35(4): 364–368, doi: 10.1016/j.apnu.2021.05.006.
27.
Almeida M., Shrestha A.D., Stojanac D., Miller L.J. The impact of the COVID-19 pandemic on women’s mental health. Arch. Womens Ment. Health 2020; 23(6): 741–748, doi: 10.1007/s00737-020-01092-2.
28.
Svensson E. Construction of a single global scale for multi-item assessments of the same variable. Stat. Med. 2001; 20(24): 3831–3846, doi: 10.1002/sim.1148.
29.
Dourado G.B., Volpato G.H., de Almeida-Pedrin R.R., Pedron Oltramari P.V., Freire Fernandes T.M., de Castro Ferreira Conti A.C. Likert scale vs visual analog scale for assessing facial pleasantness. Am. J. Orthod. Dentofacial Orthop. 2021; 160(6): 844–852, doi: 10.1016/j.ajodo.2020.05.024.
30.
Rashidi Fakari F., Simbar M. Coronavirus pandemic and worries during pregnancy; a letter to editor. Arch. Acad. Emerg. Med. 2020; 8(1): e21.
31.
Preis H., Mahaffey B., Heiselman C., Lobel M. Pandemic-related pregnancy stress and anxiety among women pregnant during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. MFM 2020; 2(3): 100155, doi: 10.1016/j.ajogmf.2020.100155.
32.
Satici B., Saricali M., Satici S.A., Griffiths M.D. Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Int. J. Ment. Health Addict. 2022; 20(5): 2731–2742, doi: 10.1007/s11469-020-00305-0.
33.
Shrivastava S.R., Shrivastava P.S. COVID-19 and impairment of mental health: public health perspective. Afr. Health Sci. 2021; 21(4): 1527–1532, doi: 10.4314/ahs.v21i4.5.
34.
Salehi L., Rahimzadeh M., Molaei E., Zaheri H., Esmaelzadeh-Saeieh S. The relationship among fear and anxiety of COVID‐19, pregnancy experience, and mental health disorder in pregnant women: A structural equation model. Brain Behav. 2020; 10(11): e01835, doi: 10.1002/brb3.1835.
35.
El Taha L., Beyrouthy C., Tamim H., Ghazeeri G. Knowledge and attitudes among Lebanese pregnant women and women seeking fertility treatment during the COVID-19 outbreak: a cross-sectional survey. BMJ Open 2022; 12(3): e057873, doi: 10.1136/bmjopen-2021-057873.
36.
Theuring S., Kengonzi A., Hafermann L., Herrmann C., Kabwama S.N., Rubaihayo J. Repercussions of the COVID-19 response in pregnant women in Western Uganda: knowledge, behavior, and emotional state after the first lockdown in 2020. Int. J. Environ. Res. Public Health 2021; 18(15): 7817, doi: 10.3390/ijerph18157817.
37.
Carleton R.N. Fear of the unknown: One fear to rule them all? J. Anxiety Disord. 2016; 41: 5–21, doi: 10.1016/j.janxdis.2016.03.011.
38.
Mizrak Sahin B., Kabakci E.N. The experiences of pregnant women during the COVID-19 pandemic in Turkey: A qualitative study. Women Birth 2021; 34(2): 162–169, doi: 10.1016/j.wombi.2020.09.022.
39.
Ilska M., Kołodziej-Zaleska A., Brandt-Salmeri A., Preis H., Lobel M. Pandemic stress and its correlates among pregnant women during the second wave of COVID-19 in Poland. Int. J. Environ. Res. Public Health 2021; 18(21): 11140, doi: 10.3390/ijerph182111140.
40.
Tomsis Y., Perez E., Sharabi L., Shaked M., Haze S., Hadid S. Postpartum post-traumatic stress symptoms following cesarean section—the mediating effect of sense of control. Psychiatr. Q. 2021; 92(4): 1839–1853, doi: 10.1007/s11126-021-09949-0.
41.
Chen H.H., Lai J.C., Hwang S.J., Huang N., Chou Y.J., Chien L.Y. Understanding the relationship between cesarean birth and stress, anxiety, and depression after childbirth: A nationwide cohort study. Birth 2017; 44(4): 369–376, doi: 10.1111/birt.12295.
42.
Saccone G., Florio A., Aiello F., Venturella R., De Angelis M.C., Locci M. et al. Psychological impact of coronavirus disease 2019 in pregnant women. Am. J. Obstet. Gynecol. 2020; 223(2): 293–295, doi: 10.1016/j.ajog.2020.05.003.
43.
Di Toro F., Gjoka M., Di Lorenzo G., De Santo D., De Seta F., Maso G. et al. Impact of COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin. Microbiol. Infect. 2021; 27(1): 36–46, doi: 10.1016/j.cmi.2020.10.007.
44.
Pichler-Stachl E., Pichler G., Baik N., Urlesberger B., Alexander A., Urlesberger P. et al. Maternal stress after preterm birth: Impact of length of antepartum hospital stay. Women Birth 2016; 29(6): e105–e109, doi: 10.1016/j.wombi.2016.04.008.
45.
Chhari N., Mehta S.C. Stress among patients during hospitalization: A study from Central India. Natl. J. Community Med. 2016; 7(4): 274–277.
46.
Akgor U., Fadıloglu E., Soyak B., Unal C., Cagan M., Temiz B.E. et al. Anxiety, depression and concerns of pregnant women during the COVID-19 pandemic. Arch. Gynecol. Obstet. 2021; 304(1): 125–130, doi: 10.1007/s00404-020-05944-1.
47.
Liu J.M., Chiu F.H., Liu Y.P., Chen S.P., Chan H.H., Yang J.J. et al. Antepartum urinary tract infection and postpartum depression in Taiwan – a nationwide population-based study. BMC Pregnancy Childbirth 2018; 18(1): 79, doi: 10.1186/s12884-018-1692-6.
48.
Farkash E., Weintraub A.Y., Sergienko R., Wiznitzer A., Zlotnik A., Sheiner E. Acute antepartum pyelonephritis in pregnancy: a critical analysis of risk factors and outcomes. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012; 162(1): 24–27, doi: 10.1016/j.ejogrb.2012.01.024.
49.
Verhoeven C.J.M., Boer J., Kok M., Nieuwenhuijze M., de Jonge A., Peters L.L. More home births during the COVID‐19 pandemic in the Netherlands. Birth 2022; 49(4): 792–804, doi: 10.1111/birt.12646.
50.
Cheng R.J., Fisher A.C., Nicholson S.C. Interest in home birth during the COVID‐19 pandemic: Analysis of Google Trends data. J. Midwifery Womens Health 2022; 67(4): 427–434, doi: 10.1111/jmwh.13341.
51.
de Jonge A., Baron R., Westerneng M., Twisk J., Hutton E.K. Perinatal mortality rate in the Netherlands compared to other European countries: a secondary analysis of Euro-PERISTAT data. Midwifery 2013; 29(8): 1011–1018, doi: 10.1016/j.midw.2013.02.005.
52.
Gdańska P., Drozdowicz-Jastrzębska E., Grzechocińska B., Radziwon-Zaleska M., Węgrzyn P., Wielgoś M. Anxiety and depression in women undergoing infertility treatment. Ginekol. Pol. 2017; 88(2): 109–112, doi: 10.5603/GP.a2017.0019.
53.
Kang Y.T., Yao Y., Dou J., Guo X., Li S.Y., Zhao C.N. et al. Prevalence and risk factors of maternal anxiety in late pregnancy in China. Int. J. Environ. Res. Public Health 2016; 13(5): 468, doi: 10.3390/ijerph13050468.
54.
Marquesim N.A., Cavassini A.C., Morceli G., Magalhães C.G., Rudge M.V., Calderon Ide M. et al. Depression and anxiety in pregnant women with diabetes or mild hyperglycemia. Arch. Gynecol. Obstet. 2016; 293(4): 833–837, doi: 10.1007/s00404-015-3838-3.
55.
Jin X., Cheng Z., Yu X., Tao Q., Huang R., Wang S. Continuous supplementation of folic acid in pregnancy and the risk of perinatal depression – A meta-analysis. J. Affect. Disord. 2022; 302: 258–272, doi: 10.1016/j.jad.2022.01.080.
Share
RELATED ARTICLE
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.