Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Mobile phone applications used to monitor age-related macular degeneration
1
Department of Health Economics and Health Management, Faculty of Public Health in Bytom, Medical University of Silesia, Katowice, Poland
2
Ophthalmology Department, District Municipal Hospital in Ruda Slaska, Poland
Corresponding author
Anna Rogalska
Zakład Ekonomiki i Zarządzania w Ochronie Zdrowia, Wydział Zdrowia Publicznego w Bytomiu, ul. Piekarska 18, 41-902 Bytom
Zakład Ekonomiki i Zarządzania w Ochronie Zdrowia, Wydział Zdrowia Publicznego w Bytomiu, ul. Piekarska 18, 41-902 Bytom
Ann. Acad. Med. Siles. 2025;79:17-23
KEYWORDS
age-related macular degenerationAMDmobile appe-health in ophthalmologymobile patient monitoringmobile healthusability evaluation
TOPICS
ABSTRACT
Introduction:
Age-related macular degeneration (AMD) is a leading cause of vision loss among elderly individuals. The aim of the study was to analyze the practical value of available mobile applications used to monitor AMD.
Material and methods:
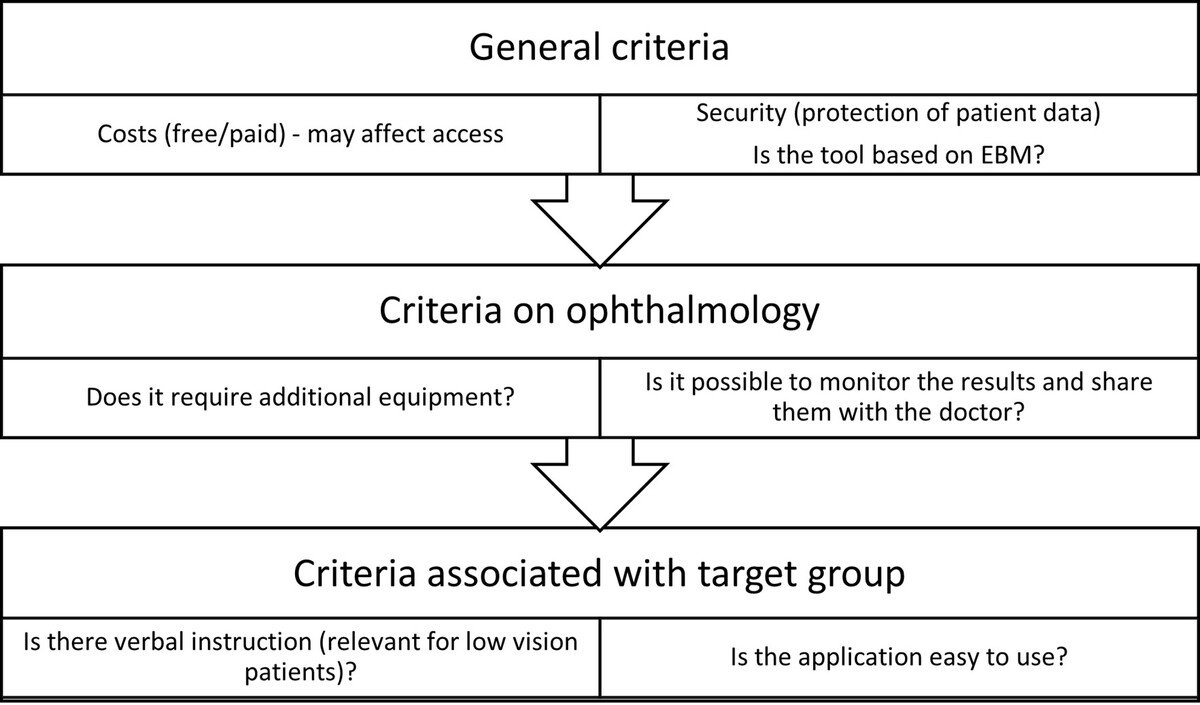
Between March 1–31, 2023, a quantitative and qualitative analysis of smartphone applications – available in Polish and English in the Google Play Store – was conducted using the keywords “age-related macular degeneration” and “AMD”. The analysis included four qualitative criteria, scored on a scale of 0–2 points each: 1) disease monitoring capability, 2) user data protection, 3) availability of verbal instructions, and 4) application usability. Based on the total scores, the applications were classified into five quality levels: very high (8 pts), high (7 pts), medium (6 pts), below medium (5 pts), and low (≤ 4 pts). An ophthalmologist tested each app that met the inclusion criteria.
Results:
Of the 249 identified applications, only 14 met the inclusion criteria for analysis. Among these, two were classified as very high quality, three as high quality (none of which were in Polish), one as medium quality, and eight as low quality. Only two out of the 14 applications addressed AMD patients’ needs, such as vision limitations and the use of verbal instructions.
Conclusions:
The available applications in Polish offered no added value over the traditional paper-based Amsler test. For mobile applications to effectively aid in AMD monitoring, key aspects such as availability (preferably free) and quality, including data security, should be prioritized. Creating evaluation teams that include medical experts, IT specialists, and patient representatives would enhance the development and assessment of AMD-focused mobile applications.
Age-related macular degeneration (AMD) is a leading cause of vision loss among elderly individuals. The aim of the study was to analyze the practical value of available mobile applications used to monitor AMD.
Material and methods:
Between March 1–31, 2023, a quantitative and qualitative analysis of smartphone applications – available in Polish and English in the Google Play Store – was conducted using the keywords “age-related macular degeneration” and “AMD”. The analysis included four qualitative criteria, scored on a scale of 0–2 points each: 1) disease monitoring capability, 2) user data protection, 3) availability of verbal instructions, and 4) application usability. Based on the total scores, the applications were classified into five quality levels: very high (8 pts), high (7 pts), medium (6 pts), below medium (5 pts), and low (≤ 4 pts). An ophthalmologist tested each app that met the inclusion criteria.
Results:
Of the 249 identified applications, only 14 met the inclusion criteria for analysis. Among these, two were classified as very high quality, three as high quality (none of which were in Polish), one as medium quality, and eight as low quality. Only two out of the 14 applications addressed AMD patients’ needs, such as vision limitations and the use of verbal instructions.
Conclusions:
The available applications in Polish offered no added value over the traditional paper-based Amsler test. For mobile applications to effectively aid in AMD monitoring, key aspects such as availability (preferably free) and quality, including data security, should be prioritized. Creating evaluation teams that include medical experts, IT specialists, and patient representatives would enhance the development and assessment of AMD-focused mobile applications.
FUNDING
No specific grant was received for this study.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
REFERENCES (40)
1.
Fleckenstein M., Keenan T.D.L., Gfuymer R.H., Chakravarthy U., Schmitz-Valckenberg S., Klaver C.C. et al. Age-related macular degeneration. Nat. Rev. Dis. Primers 2021; 7(1): 31, doi: 10.1038/s41572-021-00265-2.
2.
Age-Related Macular Degeneration (AMD). National Eye Institute, 2021 [online] https://www.nei.nih.gov/learn-... [accessed on 14 September 2023].
3.
Keenan T.D.L., Cukras C.A., Chew E.Y. Age-related macular degeneration: epidemiology and clinical aspects. Adv. Exp. Med. Biol. 2021; 1256: 1–31, doi: 10.1007/978-3-030-66014-7_1.
4.
Ayoub T., Patel N. Age-related macular degeneration. J. R. Soc. Med. 2009; 102(2): 56–61, doi: 10.1258/jrsm.2009.080298.
5.
Wong W.L., Su X., Li X., Cheung C.M., Klein R., Cheng C.Y. et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob. Health 2014; 2(2): e106–116, doi: 10.1016/S2214-109X(13)70145-1.
6.
Lambert N.G., ElShelmani H., Singh M.K., Mansergh F.C., Wride M.A., Padilla M. et al. Risk factors and biomarkers of age-related macular degeneration. Prog. Retin. Eye Res. 2016; 54: 64–102, doi: 10.1016/j.preteyeres.2016.04.003.
7.
Fritsche L.G., Igl W., Bailey J.N., Grassmann F., Sengupta S., Bragg-Gresham J.L. et al. A large genome-wide association study of age-related macular degeneration highlights contributions of rare and common variants. Nat. Genet. 2016; 48(2): 134–143, doi: 10.1038/ng.3448.
8.
Pennington K.L., DeAngelis M.M. Epidemiology of age-related macular degeneration (AMD): associations with cardiovascular disease phenotypes and lipid factors. Eye Vis. (Lond.) 2016; 3: 34, doi: 10.1186/s40662-016-0063-5.
9.
Heesterbeek T.J. Lorés-Motta L., Hoyng C.B., Lechanteur Y.T.E., den Hollander A.I. Risk factors for progression of age-related macular degeneration. Ophthalmic Physiol. Opt. 2020; 40(2): 140–170, doi: 10.1111/opo.12675.
10.
Shim S.H., Kim S.G., Bae J.H., Yu H.G., Song S.J. et al. Risk factors for progression of early age-related macular degeneration in Koreans. Ophthalmic Epidemiol. 2016; 23(2): 80–87, doi: 10.3109/09286586.2015.1129425.
11.
Merle B.M.J., Colijn J.M., Cougnard-Grégoire A., de Koning-Backus A.P.M., Delyfer M.N., Kiefte-de Jong J.C. et al. Mediterranean diet and incidence of advanced age-related macular degeneration: The EYE-RISK Consortium. Ophthalmology 2019; 126(3): 381–390, doi: 10.1016/j.ophtha.2018.08.006.
12.
Merle B.M., Silver R.E., Rosner B., Seddon J.M. Adherence to a Mediterranean diet, genetic susceptibility, and progression to advanced macular degeneration: a prospective cohort study. Am. J. Clin. Nutr. 2015; 102(5): 1196–1206, doi: 10.3945/ajcn.115.111047.
13.
Coronado B.N.L., da Cunha F.B.S., de Oliveira R.M., Nóbrega O.T., Ricart C.A.O., Fontes W. et al. Novel possible protein targets in neovascular age-related macular degeneration: a pilot study experiment. Front. Med. (Lausanne) 2021; 8: 692272, doi: 10.3389/fmed.2021.692272.
14.
Gu B.J., Huang X., Avula P.K., Caruso E., Drysdale C., Vessey K.A. et al. Deficits in monocyte function in age related macular degeneration: a novel systemic change associated with the disease. Front. Med. (Lausanne) 2021; 8: 634177, doi: 10.3389/fmed.2021.634177.
15.
VanDenLangenberg A.M., Carson M.P. Drusen Bodies. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing 2023, [online] https://www.ncbi.nlm.nih.gov/b... [accessed on 14 September 2024].
16.
Ayhan I., Doyle E., Zanker J. Measuring image distortions arising from age-related macular degeneration: An Iterative Amsler Grid (IAG). MedComm. (2020) 2022; 3(1): e107, doi: 10.1002/mco2.107.
17.
Sim S.S., Yip M.Y., Wang Z., Tan A.C.S., Tan G.S.W., Cheung C.M.G. et al. Digital technology for AMD management in the post-COVID-19 new normal. Asia Pac. J. Ophthalmol. (Phila.) 2021; 10(1): 39–48, doi: 10.1097/APO.0000000000000363.
18.
Crossland M., Rubin G. The Amsler chart: absence of evidence is not evidence of absence. Br. J. Ophthalmol. 2007; 91(3): 391–393, doi: 10.1136/bjo.2006.095315.
19.
Choritz L., Hoffmann M., Thieme H. Telemedical applications in ophthalmology in times of COVID-19. [Article in German]. Ophthalmologe 2021; 118(9): 885–892, doi: 10.1007/s00347-021-01470-w.
20.
Dorsey E.R., Topol E.J. State of telehealth. N. Engl. J. Med. 2016; 375(14): 1400, doi: 10.1056/NEJMc1610233.
21.
Gioia G., Salducci M. Medical and legal aspects of telemedicine in ophthalmology. Rom. J. Ophthalmol. 2019; 63(3): 197–207.
22.
Gupta A., Cavallerano J., Sun J.K., Silva P.S. Evidence for telemedicine for diabetic retinal disease. Semin. Ophthalmol. 2017; 32(1): 22–28, doi: 10.1080/08820538.2016.1228403.
23.
Sharma M., Jain N., Ranganathan S., Sharma N., Honavar S.G., Sharma N. et al. Tele-ophthalmology: Need of the hour. Indian J. Ophthalmol. 2020; 68(7): 1328–1338, doi: 10.4103/ijo.IJO_1784_20.
24.
Liu Y., Zupan N.J., Swearingen R., Jacobson N., Carlson J.N., Mahoney J.E. et al. Identification of barriers, facilitators and system-based implementation strategies to increase teleophthalmology use for diabetic eye screening in a rural US primary care clinic: a qualitative study. BMJ Open 2019; 9(2): e022594, doi: 10.1136/bmjopen-2018-022594.
25.
Mansberger S.L., Sheppler C., Barker G., Gardiner S.K., Demirel S. et al. Long-term comparative effectiveness of telemedicine in providing diabetic retinopathy screening examinations: a randomized clinical trial. JAMA Ophthalmol. 2015; 133(5): 518–525, doi: 10.1001/jamaophthalmol.2015.1.
26.
Agarwal P., Gordon D., Griffith J., Kithulegoda N., Witteman H.O., Sacha Bhatia R. et al. Assessing the quality of mobile applications in chronic disease management: a scoping review. NPJ Digit. Med. 2021; 4(1): 46, doi: 10.1038/s41746-021-00410-x.
27.
Liew M.S., Zhang J., See J., Ong Y.L. Usability challenges for health and wellness mobile apps: mixed-methods study among mHealth experts and consumers. JMIR Mhealth Uhealth 2019; 7(1): e12160, doi: 10.2196/12160.
28.
Skrzypecki J., Stanska K., Grabska-Liberek I. Patient-oriented mobile applications in ophthalmology. Clin. Exp. Optom. 2019; 102(2): 180–183, doi: 10.1111/cxo.12830.
29.
Lombardo M., Serrao S., Lombardo G. Challenges in Age-related macular degeneration: from risk factors to novel diagnostics and prevention strategies. Front. Med. (Lausanne) 2022; 9: 887104, doi: 10.3389/fmed.2022.887104.
30.
Hamine S., Gerth-Guyette E., Faulx D., Green B.B., Ginsburg A.S. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J. Med. Internet Res. 2015; 17(2): e52, doi: 10.2196/jmir.3951.
31.
Llorens-Vernet P., Miró J. The Mobile App Development and Assessment Guide (MAG): Delphi-based validity study. JMIR Mhealth Uhealth 2020; 8(7): e17760, doi: 10.2196/17760.
32.
Huckvale K., Prieto J.T., Tilney M., Benghozi P.J., Car J. Unaddressed privacy risks in accredited health and wellness apps: a cross-sectional systematic assessment. BMC Med. 2015; 13: 214, doi: 10.1186/s12916-015-0444-y.
33.
Byambasuren O., Sanders S., Beller E., Glasziou P. Prescribable mHealth apps identified from an overview of systematic reviews. NPJ Digit. Med. 2018; 1: 12, doi: 10.1038/s41746-018-0021-9.
34.
Khurana R.N., Hoang C., Khanani A.M., Steklov N., Singerman L.J. A smart mobile application to monitor visual function in diabetic retinopathy and age-related macular degeneration: The CLEAR study. Am. J. Ophthalmol. 2021; 227: 222–230, doi: 10.1016/j.ajo.2021.03.033.
35.
Yu H.J., Kiernan D.F., Eichenbaum D., Sheth V.S., Wykoff C.C. Home monitoring of age-related macular degeneration: utility of the ForeseeHome device for detection of neovascularization. Ophthalmol. Retina 2021; 5(4): 348–356, doi: 10.1016/j.oret.2020.08.003.
36.
Schmid M.K. Thiel M.A., Lienhard K., Schlingemann R.O., Faes L., Bachmann L.M. Reliability and diagnostic performance of a novel mobile app for hyperacuity self-monitoring in patients with age-related macular degeneration. Eye (Lond.) 2019; 33(10): 1584–1589, doi:10.1038/s41433-019-0455-6.
37.
Gross N., Bachmann L.M., Islam M., Faes L., Schmid M.K., Thiel M.A. et al. Visual outcomes and treatment adherence of patients with macular pathology using a mobile hyperacuity home-monitoring app: a matched-pair analysis. BMJ Open 2021; 11(12): e056940, doi: 10.1136/bmjopen-2021-056940.
38.
Islam M., Sansome S., Das R., Lukic M., Chong Teo K.Y., Tan G. et al. Smartphone-based remote monitoring of vision in macular disease enables early detection of worsening pathology and need for intravitreal therapy. BMJ Health Care Inform. 2021; 28(1): e100310, doi: 10.1136/bmjhci-2020-100310.
39.
Chen J.S., Adelman R.A. Hyperacuity exam screens for choroidal neovascularization in age-related macular degeneration on a mobile device. Ophthalmic Surg. Lasers Imaging Retina 2016; 47(8): 708–715, doi: 10.3928/23258160-20160808-03.
40.
Tseng R.M.W.W., Tham Y.C., Rim T.H., Cheng C.Y. Emergence of non-artificial intelligence digital health innovations in ophthalmology: A systematic review. Clin. Exp. Ophthalmol. 2021; 49(7): 741–756, doi: 10.1111/ceo.13971.
CITATIONS (1):
1.
The Amsler Grid in Everyday Practice: A Review of Its Role and Limitations in Primary Care
Agata Estreicher, Kamil Biedka, Katarzyna Błaszczyk, Michał Wesołowski, Jakub Bulski, Aleksandra Sobaś, Oliwia Ziobro, Filip Maj, Karol Sornat, Anna Klasa, Kacper Żełabowski, Jakub Karwacki, Tadeusz Sebzda
Clinical Ophthalmology
Agata Estreicher, Kamil Biedka, Katarzyna Błaszczyk, Michał Wesołowski, Jakub Bulski, Aleksandra Sobaś, Oliwia Ziobro, Filip Maj, Karol Sornat, Anna Klasa, Kacper Żełabowski, Jakub Karwacki, Tadeusz Sebzda
Clinical Ophthalmology
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.