Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
The impact of common chronic diseases on the severity of clinical symptoms of COVID-19
1
Department of Medical Biophysics, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
Corresponding author
Barbara Pietrzyk
Katedra i Zakład Biofizyki Lekarskiej, Wydział Nauk Medycznych w Katowicach ŚUM, ul. Medyków 18, 40-752 Katowice
Katedra i Zakład Biofizyki Lekarskiej, Wydział Nauk Medycznych w Katowicach ŚUM, ul. Medyków 18, 40-752 Katowice
Ann. Acad. Med. Siles. 2025;79:261-268
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Most available research on the etiopathogenesis of COVID-19 predominantly focuses on adult populations with chronic diseases in advanced stages – including severe respiratory and cardiovascular disorders, as well as oncological conditions – where correlations with the clinical course of the disease have been observed. The clinical course of COVID-19 is highly variable, ranging from asymptomatic or mild manifestations to severe respiratory and circulatory failure and death. The objective of the study was to assess whether common chronic diseases influence the severity of the clinical symptoms of COVID-19.
Material and Methods:
A retrospective study was conducted on a group of 208 patients between October 2022 and February 2023. An author-designed questionnaire collected data on post-COVID-19 symptoms and their severity (mild, moderate, or severe), frequency, and links to comorbidities. Descriptive statistics were used, with significance set at p < 0.05. Comparisons of variables were made using the χ² test.
Results:
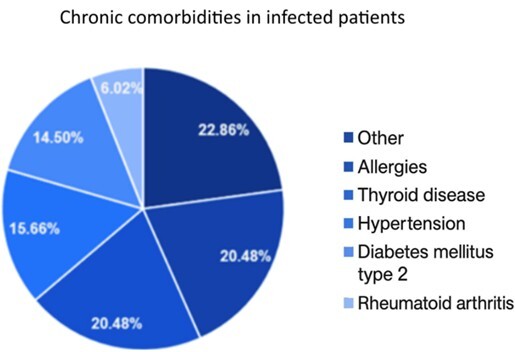
Among the patients, 50.48% had chronic diseases, of which 55% experienced mild symptoms of COVID-19 and 40% experienced moderate symptoms. In the group without chronic diseases (49.52%), mild symptoms were observed in 58% of patients and moderate symptoms in 36%. No significant correlation was found between chronic diseases and the severity of symptoms (p = 0.809).
Conclusions:
No significant correlation was found between mild chronic diseases and the severity of COVID-19 symptoms. The type, severity, and duration of the conditions and the level of viremia influence the prognosis. Further studies are needed to consider additional factors, such as gender and age.
Most available research on the etiopathogenesis of COVID-19 predominantly focuses on adult populations with chronic diseases in advanced stages – including severe respiratory and cardiovascular disorders, as well as oncological conditions – where correlations with the clinical course of the disease have been observed. The clinical course of COVID-19 is highly variable, ranging from asymptomatic or mild manifestations to severe respiratory and circulatory failure and death. The objective of the study was to assess whether common chronic diseases influence the severity of the clinical symptoms of COVID-19.
Material and Methods:
A retrospective study was conducted on a group of 208 patients between October 2022 and February 2023. An author-designed questionnaire collected data on post-COVID-19 symptoms and their severity (mild, moderate, or severe), frequency, and links to comorbidities. Descriptive statistics were used, with significance set at p < 0.05. Comparisons of variables were made using the χ² test.
Results:
Among the patients, 50.48% had chronic diseases, of which 55% experienced mild symptoms of COVID-19 and 40% experienced moderate symptoms. In the group without chronic diseases (49.52%), mild symptoms were observed in 58% of patients and moderate symptoms in 36%. No significant correlation was found between chronic diseases and the severity of symptoms (p = 0.809).
Conclusions:
No significant correlation was found between mild chronic diseases and the severity of COVID-19 symptoms. The type, severity, and duration of the conditions and the level of viremia influence the prognosis. Further studies are needed to consider additional factors, such as gender and age.
REFERENCES (39)
1.
Bajgain K.T., Badal S., Bajgain B.B., Santana M.J. Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature. Am. J. Infect. Control 2021; 49(2): 238–246, doi: 10.1016/j.ajic.2020.06.213.
2.
Booth A., Reed A.B., Ponzo S., Yassaee A., Aral M., Plans D. et al. Population risk factors for severe disease and mortality in COVID-19: A global systematic review and meta-analysis. PLoS One 2021; 16(3): e0247461, doi: 10.1371/journal.pone.0247461.
3.
Opuchlik M., Opuchlik A.M., Żurawski A., Zabojszcz M., Biskup M., Markowski K. et al. Complications after COVID-19 – review of scientific reports and meta-analysis. Medical Studies/Studia Medyczne 2024; 40(2): 225–239, doi: 10.5114/ms.2024.140984.
4.
Zhang J.J., Dong X., Liu G.H., Gao Y.D. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin. Rev. Allergy Immunol. 2023; 64(1): 90–107, doi: 10.1007/s12016-022-08921-5.
5.
Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R. et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020; 172(9): 577–582, doi: 10.7326/M20-0504.
6.
Bean J., Kuri-Cervantes L., Pennella M., Betts M.R., Meyer N.J., Hassan W.M. Multivariate indicators of disease severity in COVID-19. Sci. Rep. 2023; 13(1): 5145, doi: 10.1038/s41598-023-31683-9.
7.
Mattiuzzi C., Lippi G. Timeline analysis of clinical severity of COVID-19 in the general population. Eur. J. Intern. Med. 2023; 110: 97–98, doi: 10.1016/j.ejim.2022.12.007.
8.
Kim G.U., Kim M.J., Ra S.H., Lee J., Bae S., Jung J. et al. Clinical characteristics of asymptomatic and symptomatic patients with mild COVID-19. Clin. Microbiol. Infect. 2020; 26(7): 948.e1–948.e3, doi: 10.1016/j.cmi.2020.04.040.
9.
da Costa E Silva G.R., Moura W.É.A., Dos Santos K.C., Gomes D.O., Bandeira G.N., Guimarães R.A. et al. Long-term symptoms after mild coronavirus disease in healthy healthcare professionals: A 12-month prospective cohort study. Int. J. Environ. Res. Public Health 2023; 20(2): 1483, doi: 10.3390/ijerph20021483.
10.
Narang K., Miller M., Trinidad C., Wick M., Theiler R., Weaver A.L. et al. Impact of asymptomatic and mild COVID-19 infection on fetal growth during pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2023; 281: 63–67, doi: 10.1016/j.ejogrb.2022.12.020.
11.
Gandhi R.T., Lynch J.B., Del Rio C. Mild or moderate Covid-19. N. Engl. J. Med. 2020; 383(18): 1757–1766, doi: 10.1056/NEJMcp2009249.
12.
Bernell S., Howard S.W. Use your words carefully: What is a chronic disease? Front. Public Health 2016; 4: 159, doi: 10.3389/fpubh.2016.00159.
13.
Sepúlveda-Loyola W., Rodríguez-Sánchez I., Pérez-Rodríguez P., Ganz F., Torralba R., Oliveira D.V. et al. Impact of social isolation due to COVID-19 on health in older people: Mental and physical effects and recommendations. J. Nutr. Health Aging 2020; 24(9): 938–947, doi: 10.1007/s12603-020-1500-7.
14.
Mahumud R.A., Kamara J.K., Renzaho A.M.N. The epidemiological burden and overall distribution of chronic comorbidities in coronavirus disease-2019 among 202,005 infected patients: evidence from a systematic review and meta-analysis. Infection 2020; 48(6): 813–833, doi: 10.1007/s15010-020-01502-8.
15.
Shibata S., Arima H., Asayama K., Hoshide S., Ichihara A., Ishimitsu T. et al. Hypertension and related diseases in the era of COVID-19: a report from the Japanese Society of Hypertension Task Force on COVID-19. Hypertens. Res. 2020; 43(10): 1028–1046, doi: 10.1038/s41440-020-0515-0.
16.
Sun Y., Guan X., Jia L., Xing N., Cheng L., Liu B. et al. Independent and combined effects of hypertension and diabetes on clinical outcomes in patients with COVID-19: A retrospective cohort study of Huoshen Mountain Hospital and Guanggu Fangcang Shelter Hospital. J. Clin. Hypertens. 2021; 23(2): 218–231, doi: 10.1111/jch.14146.
17.
Gallo G., Calvez V., Savoia C. Hypertension and COVID-19: Current evidence and perspectives. High Blood Press. Cardiovasc. Prev. 2022; 29(2): 115–123, doi: 10.1007/s40292-022-00506-9.
18.
Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E. et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584(7821): 430–436, doi: 10.1038/s41586-020-2521-4.
19.
Rosenthal N., Cao Z., Gundrum J., Sianis J., Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Netw. Open. 2020; 3(12): e2029058, doi: 10.1001/jamanetworkopen.2020.29058.
20.
Tadic M., Cuspidi C., Grassi G., Mancia G. COVID-19 and arterial hypertension: Hypothesis or evidence? J. Clin. Hypertens. 2020; 22(7): 1120–1126, doi: 10.1111/jch.13925.
21.
Tadic M., Saeed S., Grassi G., Taddei S., Mancia G., Cuspidi C. Hypertension and COVID-19: Ongoing controversies. Front. Cardiovasc. Med. 2021; 8: 639222, doi: 10.3389/fcvm.2021.639222.
22.
El-Battrawy I., Nuñez-Gil I.J., Abumayyaleh M., Estrada V., Manuel Becerra-Muñoz V., Uribarri A. et al. COVID-19 and the impact of arterial hypertension-An analysis of the international HOPE COVID-19 Registry (Italy-Spain-Germany). Eur. J. Clin. Invest. 2021; 51(11): e13582, doi: 10.1111/eci.13582.
23.
Shalaeva E.V., Shadmanov A.K, Azizova F.L., Mirakhmedova K.T., Messerli F.H., Franco O.H. et al. Is lone hypertension a risk factor for more severe COVID-19 outcomes? Glob. Heart 2022; 17(1): 17, doi: 10.5334/gh.1099.
24.
Yoshihara F. Association between blood pressure and COVID-19 severity. Hypertens. Res. 2024; 47(3): 683–684, doi: 10.1038/s41440-023-01557-8.
25.
Drucker D.J. Diabetes, obesity, metabolism, and SARS-CoV-2 infection: the end of the beginning. Cell. Metab. 2021; 33(3): 479–498, doi: 10.1016/j.cmet.2021.01.016.
26.
Al-Kuraishy H.M., Al-Gareeb A.I., Alblihed M., Guerreiro S.G., Cruz-Martins N., Batiha G.E. COVID-19 in relation to hyperglycemia and diabetes mellitus. Front. Cardiovasc. Med. 2021; 8: 644095, doi: 10.3389/fcvm.2021.644095.
27.
Dandona P., Aljada A., Bandyopadhyay A. The potential therapeutic role of insulin in acute myocardial infarction in patients admitted to intensive care and in those with unspecified hyperglycemia. Diabetes Care 2003; 26(2): 516–519, doi: 10.2337/diacare.26.2.516.
28.
Maddaloni E., Buzzetti R. Covid-19 and diabetes mellitus: unveiling the interaction of two pandemics. Diabetes Metab. Res. Rev. 2020; 36(7): e33213321, doi: 10.1002/dmrr.3321.
29.
Kaminska H., Szarpak L., Kosior D., Wieczorek W., Szarpak A., Al-Jeabory M. Impact of diabetes mellitus on in-hospital mortality in adult patients with COVID-19: a systematic review and meta-analysis. Acta Diabetol. 2021; 58(8): 1101–1110, doi: 10.1007/s00592-021-01701-1.
30.
Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S. et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020; 180(7): 934–943, doi: 10.1001/jamainternmed.2020.0994.
31.
Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395(10229): 1054–1062, doi: 10.1016/S0140-6736(20)30566-3.
32.
Liu H., Chen S., Liu M., Nie H., Lu H. Comorbid chronic diseases are strongly correlated with disease severity among COVID-19 patients: A systematic review and meta-analysis. Aging Dis. 2020; 11(3): 668–678, doi: 10.14336/AD.2020.0502.
33.
Guan W.J, Liang W.H., Zhao Y., Liang H.R., Chen Z.S., Li Y.M. et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur. Respir. J. 2020; 55(5): 2000547, doi: 10.1183/13993003.00547-2020.
34.
Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 2020; 323(16): 1574–1581, doi: 10.1001/jama.2020.5394.
35.
Szarpak L., Mierzejewska M., Jurek J., Kochanowska A., Gasecka A., Truszewski Z. et al. Effect of coronary artery disease on COVID-19 – prognosis and risk assessment: A systematic review and meta-analysis. Biology 2022; 11(2): 221, doi: 10.3390/biology11020221.
36.
Sunjaya A.P., Allida S.M., Di Tanna G.L., Jenkins C. Asthma and risk of infection, hospitalization, ICU admission and mortality from COVID-19: Systematic review and meta-analysis. J. Asthma 2022; 59(5): 866–879, doi: 10.1080/02770903.2021.1888116.
37.
Terry P.D., Heidel R.E., Dhand R. Asthma in adult patients with COVID-19: Prevalence and risk of severe disease. Am. J. Respir. Crit. Care Med. 2021; 203(7): 893–905, doi: 10.1164/rccm.202008-3266OC.
38.
Singh D., Mathioudakis A.G., Higham A. Chronic obstructive pulmonary disease and COVID-19: interrelationships. Curr. Opin. Pulm. Med. 2022; 28(2): 76–83, doi: 10.1097/MCP.0000000000000834.
39.
Chuang H.J., Lin C.W., Hsiao M.Y., Wang T.G., Liang H.W. Long COVID and rehabilitation. J. Formos. Med. Assoc. 2024; 123 Suppl 1: S61–S69, doi: 10.1016/j.jfma.2023.03.022.
Share
RELATED ARTICLE
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.