Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
The impact of interpersonal relationships on mental health of Polish medical students
1
Students’ Scientific Club, Department of Environmental Medicine and Epidemiology, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland
2
Department of Environmental Medicine and Epidemiology, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland
Corresponding author
Janusz Kasperczyk
Katedra i Zakład Medycyny i Epidemiologii Środowiskowej, Wydział Nauk Medycz-nych w Zabrzu, Śląski Uniwersytet Medyczny w Katowicach, ul. Jordana 19, 41-808 Zabrze
Katedra i Zakład Medycyny i Epidemiologii Środowiskowej, Wydział Nauk Medycz-nych w Zabrzu, Śląski Uniwersytet Medyczny w Katowicach, ul. Jordana 19, 41-808 Zabrze
Ann. Acad. Med. Siles. 2024;78:155-166
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Interpersonal relations significantly impact our well-being and mental health. They are also crucial among students, especially when they start living independently in a new social environment. The study aimed to determine the impact of relations on the occurrence of depression, anxiety, and drowsiness among medical students in Poland.
Material and methods:
An online questionnaire was created, consisting of four parts: the authors’ questionnaire on interpersonal relations, the Beck Depression Inventory (BDI), the Generalized Anxiety Disorder 7-item Scale (GAD-7), and the Epworth Sleepiness Scale (ESS). The results were analyzed using STATISTICA software.
Results:
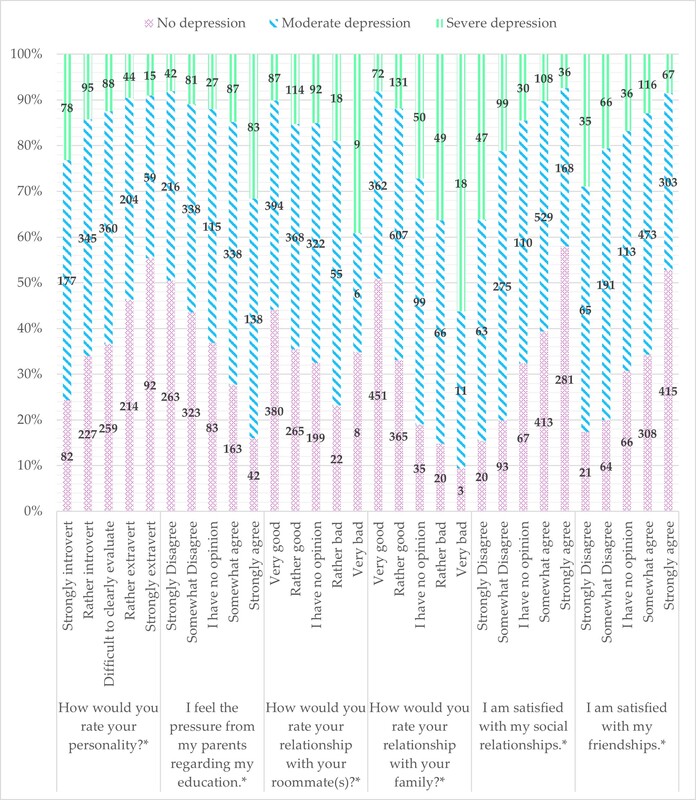
2339 completed questionnaires were obtained. 69.75% of the subjects had good/rather good relations with their co-tenants, and 5.04% – had bad/definitely bad. 85% of the participants had good relations with their parents. 65.63% of the respondents were satisfied with their social relationships; in addition, 71.91% of respondents were satisfied with their relationships with their friends. Poor relations with family and co-tenants, and poor social and friend relationships were linked to higher levels of depression, anxiety, and sleepiness. This phenomenon was particularly evident among introverts.
Conclusions:
Identifying the risk factors could significantly improve the prevention, diagnosis, and treatment of mental disorders in this group. Supporting students and paying greater attention to social competencies equally with medical knowledge acquired by them would be highly recommended.
Interpersonal relations significantly impact our well-being and mental health. They are also crucial among students, especially when they start living independently in a new social environment. The study aimed to determine the impact of relations on the occurrence of depression, anxiety, and drowsiness among medical students in Poland.
Material and methods:
An online questionnaire was created, consisting of four parts: the authors’ questionnaire on interpersonal relations, the Beck Depression Inventory (BDI), the Generalized Anxiety Disorder 7-item Scale (GAD-7), and the Epworth Sleepiness Scale (ESS). The results were analyzed using STATISTICA software.
Results:
2339 completed questionnaires were obtained. 69.75% of the subjects had good/rather good relations with their co-tenants, and 5.04% – had bad/definitely bad. 85% of the participants had good relations with their parents. 65.63% of the respondents were satisfied with their social relationships; in addition, 71.91% of respondents were satisfied with their relationships with their friends. Poor relations with family and co-tenants, and poor social and friend relationships were linked to higher levels of depression, anxiety, and sleepiness. This phenomenon was particularly evident among introverts.
Conclusions:
Identifying the risk factors could significantly improve the prevention, diagnosis, and treatment of mental disorders in this group. Supporting students and paying greater attention to social competencies equally with medical knowledge acquired by them would be highly recommended.
FUNDING
This research received no external funding. The authors have no relevant financial or non-financial interests to disclose.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
REFERENCES (67)
2.
Yoch M., Sirull R. New Global Burden of Disease analyses show depression and anxiety among the top causes of health loss worldwide, and a significant increase due to the COVID-19 pandemic. IHME, October 8, 2021 [online] https://www.healthdata.org/act... [accessed February 6, 2023].
3.
Rotenstein, L.S., Ramos M.A., Torre M., Segal J.B., Peluso M.J., Guille C. et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA 2016; 316(21): 2214–2236, doi: 10.1001/jama.2016.17324.
4.
Quek T.T., Tam W.W., Tran B.X., Zhang M., Zhang Z., Ho C.S. et al. The global prevalence of anxiety among medical students: a meta-analysis. Int. J. Environ. Res. Public Health 2019; 16(15): 2735, doi: 10.3390/ijerph16152735.
5.
Jahrami H., Alshomili H., Almannai N., Althani N., Aloffi A., Algahtani H. et al. Predictors of excessive daytime sleepiness in medical students: a meta-regression. Clocks Sleep 2019; 1(2): 209–219, doi: 10.3390/clockssleep1020018.
6.
Brenneisen Mayer F., Souza Santos I., Silveira P.S., Itaqui Lopes M.H., de Souza A.R., Campos E.P. et al. Factors associated to depression and anxiety in medical students: a multicenter study. BMC Med. Educ. 2016; 16(1): 282, doi: 10.1186/s12909-016-0791-1.
7.
Tempski P., Bellodi P.L., Paro H.B., Enns S.C., Martins M.A., Schraiber L.B. What do medical students think about their quality of life? A qualitative study. BMC Med. Educ. 2012; 12(1): 106, doi: 10.1186/1472-6920-12-106.
8.
Shao R., He P., Ling B., Tan L., Xu L., Hou Y. et al. Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol. 2020; 8(1): 38, doi: 10.1186/s40359-020-00402-8.
9.
Niño García J.A., Barragán Vergel M.F., Ortiz Labrador J.A., Ochoa Vera M.E., González Olaya H.L. Factors associated with excessive daytime sleepiness in medical students of a higher education institution of Bucaramanga. Rev. Colomb. Psiquiatr. (Engl. Ed.) 2019; 48(4): 222–231, doi: 10.1016/j.rcp.2017.12.002.
10.
Yeung W.F., Chung K.F., Cy Chan T. Sleep–wake habits, excessive daytime sleepiness and academic performance among medical students in Hong Kong. Biol. Rhythm Res. 2008; 39(4): 369–377, doi: 10.1080/09291010701425124.
11.
Mirghani H.O., Ahmed M.A., Elbadawi A.S. Daytime sleepiness and chronic sleep deprivation effects on academic performance among the Sudanese medical students. J. Taibah Univ. Med. Sci. 2015; 10(4): 467–470, doi: 10.1016/j.jtumed.2015.05.003.
12.
Pallos H., Yamada N., Doi Y., Okawa M. Sleep habits, prevalence and burden of sleep disturbances among Japanese graduate students. Sleep Biol. Rhythms 2004; 2(1): 37–42, doi: 10.1111/j.1479-8425.2003.00061.x.
13.
Rajendran D., Vinod P.B., Karthika M., Prathibha M.T. Excessive daytime sleepiness in medical students. J. Evol. Med. Dent. Sci. 2018; 7(6): 747–750.
14.
Sameer H.M., Imran N., Tarar T.N., Khawaja I.S. Association of excessive daytime sleepiness with psychological distress in medical students. Prim. Care Companion CNS Disord. 2020; 22(1): 19m02531, doi: 10.4088/PCC.19m02531.
15.
Walkiewicz M., Guziak M. Availability of psychological support for medical students in Poland. Int. J. Occup. Med. Environ. Health 2021; 34(1): 87–99, doi: 10.13075/ijomeh.1896.01539.
16.
Kelly M.E., Duff H., Kelly S., McHugh Power J.E., Brennan S., Lawlor B.A. et al. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Syst. Rev. 2017; 6(1): 259, doi: 10.1186/s13643-017-0632-2.
17.
Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010; 7(7): e1000316, doi: 10.1371/journal.pmed.1000316.
18.
McDonough M.H., Beselt L.J., Daun J.T., Shank J., Culos-Reed S.N., Kronlund L.J. et al. The role of social support in physical activity for cancer survivors: a systematic review. Psychooncology 2019; 28(10): 1945–1958, doi: 10.1002/pon.5171.
19.
Pinquart M., Duberstein P.R. Associations of social networks with cancer mortality: a meta-analysis. Crit. Rev. Oncol. Hematol. 2010; 75(2): 122–137, doi: 10.1016/j.critrevonc.2009.06.003.
20.
Du L., Shi H.Y., Qian Y., Jin X.H., Li Y., Yu H.R. et al. Association between social support and suicidal ideation in patients with cancer: A systematic review and meta-analysis. Eur. J. Cancer Care 2021; 30(2): e13382, doi: 10.1111/ecc.13382.
21.
Valtorta N.K., Kanaan M., Gilbody S., Ronzi S., Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 2016; 102(13): 1009–1016, doi: 10.1136/heartjnl-2015-308790.
22.
Oliveira A.J., Rostila M., de Leon A.P., Lopes C.S. The influence of social relationships on obesity: sex differences in a longitudinal study. Obesity 2013; 21(8): 1540–1547, doi: 10.1002/oby.20286.
23.
Hutten E., Jongen E.M.M., Vos A.E.C.C., van den Hout A.J.H.C., van Lankveld J.J.D.M. Loneliness and mental health: the mediating effect of perceived social support. Int. J. Environ. Res. Public Health 2021; 18(22): 11963, doi: 10.3390/ijerph182211963.
24.
Davidson S.K., Dowrick C.F., Gunn J.M. Impact of functional and structural social relationships on two year depression outcomes: A multivariate analysis. J. Affect. Disord. 2016; 193: 274–281, doi: 10.1016/j.jad.2015.12.025.
25.
Hallgren M., Lundin A., Tee F.Y., Burström B., Forsell Y. Somebody to lean on: Social relationships predict post-treatment depression severity in adults. Psychiatry Res. 2017; 249: 261–267, doi: 10.1016/j.psychres.2016.12.060.
26.
Smith L., Hill N., Kokanovic R. Experiences of depression, the role of social support and its impact on health outcomes. J. Ment. Health 2015; 24(6): 342–346, doi: 10.3109/09638237.2014.954693.
27.
Priest J.B. Anxiety disorders and the quality of relationships with friends, relatives, and romantic partners. J. Clin. Psychol. 2013; 69(1): 78–88, doi: 10.1002/jclp.21925.
28.
LimeSurvey GmbH, Hamburg, Germany [online] http://www.limesurvey.org [accessed February 6, 2023].
29.
Beck A.T., Ward C.H., Mendelson M., Mock J., Erbaugh J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961; 4(6): 561–571, doi: 10.1001/archpsyc.1961.01710120031004.
30.
Lasa L., Ayuso-Mateos J.L., Vázquez-Barquero J.L., Dı́ez-Manrique F.J., Dowrick C.F. The use of the Beck Depression Inventory to screen for depression in the general population: a preliminary analysis. J. Affect. Disord. 2000; 57(1–3): 261–265, doi: 10.1016/s0165-0327(99)00088-9.
31.
Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006; 166(10): 1092–1097, doi: 10.1001/archinte.166.10.1092.
32.
Williams N. The GAD-7 questionnaire. Occup. Med. 2014; 64(3): 224, doi: 10.1093/occmed/kqt161.
33.
Johns M.W. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14(6): 540–545, doi: 10.1093/sleep/14.6.540.
34.
Johns M.W. Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the Epworth sleepiness scale: Failure of the MSLT as a gold standard. J. Sleep Res. 2000; 9(1): 5–11, doi: 10.1046/j.1365-2869.2000.00177.x.
35.
Cohen J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960; 20(1): 37–46, doi: 10.1177/001316446002000104.
36.
The impact of COVID-19 on mental health cannot be made light of. WHO, 16 June 2022, [online] https://www.who.int/news-room/... [accessed February 7, 2023].
37.
Thyloth M., Singh H., Subramanian V. Increasing burden of mental illnesses across the globe: current status. Ind. J. Soc. Psych. 2016; 32(3): 254–256, doi: 10.4103/0971-9962.193208.
38.
Institute for Health Metrics and Evaluation, GBD Results, 2021 [online] https://vizhub.healthdata.org/... [accessed February 6 2023].
39.
Voltmer E., Köslich-Strumann S., Voltmer J.B., Kötter T. Stress and behavior patterns throughout medical education – a six year longitudinal study. BMC Med. Educ. 2021; 21(1): 454, doi: 10.1186/s12909-021-02862-x.
40.
Tam W., Lo K., Pacheco J. Prevalence of depressive symptoms among medical students: overview of systematic reviews. Med. Educ. 2019; 53(4): 345–354, doi: 10.1111/medu.13770.
41.
Puthran R., Zhang M.W.B., Tam W.W., Ho R.C. Prevalence of depression amongst medical students: a meta-analysis. Med. Educ. 2016; 50(4): 456–468, doi: 10.1111/medu.12962.
42.
Drożak P., Duda P., Bryliński Ł., Augustowska K., Drożak M., Bura A. et al. Depression among Polish medical students and its lifestyle-linked predictors. J. Educ. Health Sport 2021; 11(7): 156–166, doi: 10.12775/JEHS.2021.11.07.014.
43.
Seweryn M., Tyrała K., Kolarczyk-Haczyk A., Bonk M., Bulska W., Krysta K. Evaluation of the level of depression among medical students from Poland, Portugal and Germany. Psychiatr. Danub. 2015; 27(Suppl 1): S216–222.
44.
Babicki M., Piotrowski P., Mastalerz-Migas A. Assessment of insomnia symptoms, quality of life, daytime sleepiness, and psychoactive substance use among Polish students: A cross-sectional online survey for years 2016–2021 before and during COVID-19 pandemic. J. Clin. Med. 2022; 11(8): 2106, doi: 10.3390/jcm11082106.
45.
Alvi T., Assad F., Ramzan M., Khan F.A. Depression, anxiety and their associated factors among medical students. J. Coll. Physicians Surg. Pak. 2010; 20(2): 122–126.
46.
Pawlaczyk M., Siembida J., Balaj K., Rajewska-Rager A. The assessment of stress level, anxiety, depressive symptoms, and defense mechanisms among Polish and English medical students. Ann. Gen. Psychiatry 2020; 19(1): 29, doi: 10.1186/s12991-020-00274-7.
47.
Mihailescu M., Neiterman E. A scoping review of the literature on the current mental health status of physicians and physicians-in-training in North America. BMC Public Health 2019; 19(1): 1363, doi: 10.1186/s12889-019-7661-9.
48.
Cuttilan A.N., Sayampanathan A.A., Ho R.C.M. Mental health issues amongst medical students in Asia: a systematic review [2000–2015]. Ann. Transl. Med. 2016; 4(4): 72, doi: 10.3978/j.issn.2305-5839.2016.02.07.
49.
Hope V., Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med. Educ. 2014; 48(10): 963–979, doi: 10.1111/medu.12512.
50.
Dyrbye L.N., Thomas M.R., Shanafelt T.D. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad. Med. 2006; 81(4): 354–373, doi: 10.1097/00001888-200604000-00009.
51.
Vollebergh W.A., Iedema J., Bijl R.V., de Graaf R., Smit F., Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Arch. Gen. Psychiatry 2001; 58(6): 597–603, doi: 10.1001/archpsyc.58.6.597.
52.
Turcio K.H., de Moraes-Melo-Neto C.L., de Caxias F.P., Goiato M.C., Dos Santos D.M., Januzzi M.S. et al. Relationship of excessive daytime sleepiness with bruxism, depression, anxiety, stress, and sex in odontology students – A cross sectional study. J. Clin. Exp. Dent. 2022; 14(6): e464–e470, doi: 10.4317/jced.59049.
53.
Shimamoto H., Suwa M., Mizuno K. Relationships between depression, daily physical activity, physical fitness, and daytime sleepiness among Japanese university students. Int. J. Environ. Res. Public Health 2021; 18(15): 8036, doi: 10.3390/ijerph18158036.
54.
Jia Q., Qu Y., Sun H., Huo H., Yin H., You D. Mental health among medical students during COVID-19: a systematic review and meta-analysis. Front. Psychol. 2022; 13: 846789, doi: 10.3389/fpsyg.2022.846789.
55.
Coentre R., Faravelli C., Figueira M.L. Assessment of depression and suicidal behaviour among medical students in Portugal. Int. J. Med. Educ. 2016; 7: 354–363, doi: 10.5116/ijme.57f8.c468.
56.
Eller T., Aluoja A., Vasar V., Veldi M. Symptoms of anxiety and depression in Estonian medical students with sleep problems. Depress. Anxiety 2006; 23(4): 250–256, doi: 10.1002/da.20166.
57.
Ghodasara S.L., Davidson M.A., Reich M.S., Savoie C.V., Rodgers S.M. Assessing student mental health at the Vanderbilt University School of Medicine. Acad. Med. 2011; 86(1): 116–121, doi: 10.1097/ACM.0b013e3181ffb056.
58.
El Hangouche A.J., Jniene A., Aboudrar S., Errguig L., Rkain H., Cherti M. et al. Relationship between poor quality sleep, excessive daytime sleepiness and low academic performance in medical students. Adv. Med. Educ. Pract. 2018; 9: 631–638, doi: 10.2147/AMEP.S162350.
59.
Mayor E. Gender roles and traits in stress and health. Front. Psychol. 2015; 6: 1–7, doi: 10.3389/fpsyg.2015.00779.
60.
Moreira de Sousa J., Moreira C.A., Telles-Correia D. Anxiety, depression and academic performance: a study amongst Portuguese medical students versus non-medical students. Acta Med. Port. 2018; 31(9): 454–462, doi: 10.20344/amp.9996.
61.
Parker G., Brotchie H. Gender differences in depression. Int. Rev. Psychiatry 2010; 22(5): 429–436, doi: 10.3109/09540261.2010.492391.
62.
Peng L., Zhang J., Li M., Li P., Zhang Y., Zuo X. et al. Negative life events and mental health of Chinese medical students: the effect of resilience, personality and social support. Psychiatry Res. 2012; 196(1): 138–141, doi: 10.1016/j.psychres.2011.12.006.
63.
Shi M., Liu L., Wang Z.Y., Wang L. The mediating role of resilience in the relationship between big five personality and anxiety among Chinese medical students: a cross-sectional study. PLoS One 2015; 10(3): e0119916, doi: 10.1371/journal.pone.0119916.
64.
Rathi A., Ransing R.S., Mishra K.K., Narula N. Quality of sleep among medical students: relationship with personality traits. JCDR 2018; 12(9): VC01–VC04, doi: 10.7860/JCDR/2018/24685.12025.
65.
Darling C.A., McWey L.M., Howard S.N., Olmstead S.B. College student stress: the influence of interpersonal relationships on sense of coherence. Stress Health J. Int. Soc. Invest. Stress 2007; 23(4): 215–229, doi: 10.1002/smi.1139.
66.
Zhang S., Li Y., Ren S., Liu T. Associations between undergraduates’ interpersonal relationships and mental health in perspective of social network analysis. Curr. Psychol. 2023; 42(14): 2059–2066, doi: 10.1007/s12144-021-01629-3.
67.
Yoon H.S., Kim G.H., Kim J. Effectiveness of an interpersonal relationship program on interpersonal relationships, self-esteem, and depression in nursing students. J. Korean. Acad. Nurs. 2011; 41(6): 805–813, doi: 10.4040/jkan.2011.41.6.805.
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.