Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Awareness of parents of preschool children about selected heavy metals in food
1
Students’ Scientific Club, Department of Environmental Health, Faculty of Public Health in Bytom, Medical University of Silesia, Katowice, Poland
2
Department of Environmental Health, Faculty of Public Health in Bytom, Medical University of Silesia, Katowice, Poland
Corresponding author
Weronika Osmala-Kurpiewska
Zakład Zdrowia Środowiskowego, Wydział Zdrowia Publicznego w Bytomiu, Śląski Uniwersytet Medyczny w Katowicach, ul. Piekarska 18, 41-902 Bytom
Zakład Zdrowia Środowiskowego, Wydział Zdrowia Publicznego w Bytomiu, Śląski Uniwersytet Medyczny w Katowicach, ul. Piekarska 18, 41-902 Bytom
Ann. Acad. Med. Siles. 2024;78:61-72
KEYWORDS
TOPICS
ABSTRACT
Introduction:
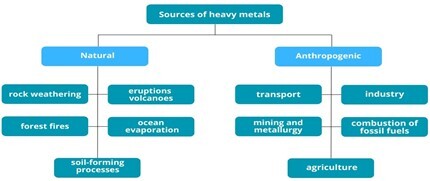
Human activity has contributed to the widespread distribution of heavy metals in the natural environment. The effects of exposure to heavy metals may not become apparent until many years later. Understanding and understanding the health risks of heavy metals in food is essential to protect children’s health. The study aimed to assess the level of knowledge about heavy metals, their occurrence in food, and the health risks to children from eating food contaminated with heavy metals.
Material and methods:
The research tool was the author’s questionnaire, consisting of the “specification” part and closed questions, mainly of a single choice. The study group consisted of 100 parents of two kindergartens located in the Silesian voivodeship. The results of the survey questionnaire were developed in Microsoft Office Excel 2019. Statistica 13 (StatSoft) was used for statistical analysis (chi-square test) and statistical significance was assumed at the level of α = 0.05.
Results:
Parents of preschool-age children are not aware of the associated risks of exposure to heavy metals. Most of the respondents did not read the general information on the presence of heavy metals in food products.
Conclusions:
The awareness of preschool-age parents about selected heavy metals in food is low. It is recommended to implement educational activities to increase the level of parental knowledge about possible health consequences and ways to reduce the health risk resulting from exposure to heavy metals through food.
Human activity has contributed to the widespread distribution of heavy metals in the natural environment. The effects of exposure to heavy metals may not become apparent until many years later. Understanding and understanding the health risks of heavy metals in food is essential to protect children’s health. The study aimed to assess the level of knowledge about heavy metals, their occurrence in food, and the health risks to children from eating food contaminated with heavy metals.
Material and methods:
The research tool was the author’s questionnaire, consisting of the “specification” part and closed questions, mainly of a single choice. The study group consisted of 100 parents of two kindergartens located in the Silesian voivodeship. The results of the survey questionnaire were developed in Microsoft Office Excel 2019. Statistica 13 (StatSoft) was used for statistical analysis (chi-square test) and statistical significance was assumed at the level of α = 0.05.
Results:
Parents of preschool-age children are not aware of the associated risks of exposure to heavy metals. Most of the respondents did not read the general information on the presence of heavy metals in food products.
Conclusions:
The awareness of preschool-age parents about selected heavy metals in food is low. It is recommended to implement educational activities to increase the level of parental knowledge about possible health consequences and ways to reduce the health risk resulting from exposure to heavy metals through food.
REFERENCES (51)
1.
Hejna M., Gottardo D., Baldi A., Dell’Orto V., Cheli F., Zaninelli M. et al. Review: Nutritional ecology of heavy metals. Animal 2018; 12(10): 2156–2170, doi: 10.1017/S175173111700355X.
2.
Kaushik P., Khandelwal R., Rawat N., Sharma M.K. Environmental hazards of heavy metal pollution and toxicity: A review. Flora and Fauna 2022; 28(2): 315–327, doi: 10.33451/florafauna.v28i2pp315-327.
3.
Witkowska D., Słowik J., Chilicka K. Heavy metals and human health: Possible exposure pathways and the competition for protein binding sites. Molecules 2021; 26(19): 6060, doi: 10.3390/molecules26196060.
4.
Ali H., Khan E., Ilahi I. Environmental chemistry and ecotoxicology of hazardous heavy metals: Environmental persistence, toxicity, and bioaccumulation. J. Chem. 2019; 2019: 6730305, doi: 10.1155/2019/6730305.
5.
Sonone S.S., Jadhav S.V., Sankhla M.S., Kumar R. Water contamination by heavy metals and their toxic effect on aquaculture and human health through food chain. Letters in Applied NanoBioScience 2021; 10(2): 2148–2166, doi: 10.33263/LIANBS102.21482166.
6.
Timothy N., Williams E.T. Environmental pollution by heavy metal: An overview. Int. J. Environ. Chem. 2019; 3(2): 72–82, doi: 10.11648/j.ijec.20190302.14.
7.
Dróżdż-Afelt J., Koim-Puchowska B.B., Menka A. Wybrane pierwiastki śladowe w organizmie człowieka. Kosmos 2019; 68(3): 503–512, doi: 10.36921/kos.2019_2461.
8.
Gut K., Marchwińska-Wyrwał E., Rogala D. Effect of preparation of carrots for consumption and content of heavy metals in the product consumed. Med. Og. Nauk Zdr. 2017; 23(4): 240–244, doi: 10.26444/monz/79282.
9.
Spychała A., Klita W., Gut K. Non-dietary exposure of children and adolescents to heavy metals in soils of recreational areas in the Silesian region – Księża Góra in Radzionków. Med. Srod. 2019; 22(3–4): 65–70, doi: 10.26444/ms/133465.
10.
Al Osman M., Yang F., Massey I.Y. Exposure routes and health effects of heavy metals on children. Biometals 2019; 32(4): 563–573, doi: 10.1007/s10534-019-00193-5.
11.
Roberts D.J., Bradberry S.M., Butcher F., Busby A. Lead exposure in children. BMJ 2022; 377: e063950, doi: 10.1136/bmj-2020-063950.
12.
Staniak S. Źródła i poziom zawartości ołowiu w żywności. Polish Journal of Agronomy 2014; 19: 36–45.
13.
Orłowska J., Pelc W., Machoń-Grecka A., Dobrakowski M., Pawlas N., Krzemień P. et al. The role of selected dietary and hygiene habits in environmental lead exposure children. Med. Srod. 2018; 21(4): 31–38, doi: 10.19243/2018404.
14.
Council on Environmental Health. Prevention of childhood lead toxicity. Pediatrics 2016; 138(1): e20161493, doi: 10.1542/peds.2016-1493.
15.
Toxicological profile for lead. Chapter 5. Potential for human exposure. ATSDR – Agency for Toxic Substances and Disease Registry [online] https://wwwn.cdc.gov/TSP/ToxPr... [accessed on 6 April 2023].
16.
Reuben A., Caspi A., Belsky D.W., Broadbent J., Harrington H., Sugden K. et al. Association of childhood blood lead levels with cognitive function and socioeconomic status at age 38 years and with IQ change and socioeco-nomic mobility between childhood and adulthood. JAMA 2017; 317(12): 1244–1251, doi: 10.1001/jama.2017.1712.
17.
Vogel N., Murawski A., Schmied-Tobies M.I.H., Rucic E., Doyle U., Kämpfe A. et al. Lead, cadmium, mercury, and chromium in urine and blood of children and adolescents in Germany – Human biomonitoring results of the German Environmental Survey 2014–2017 (GerES V). Int. J. Hyg. Environ. Health 2021; 237: 113822, doi: 10.1016/j.ijheh.2021.113822.
18.
Champion W.M., Khaliq M., Mihelcic J.R. Advancing knowledge to reduce lead exposure of children in data-poor low- and middle-income countries. Environ. Sci. Technol. Lett. 2022; 9(11): 879–888, doi: 10.1021/acs.estlett.2c00656.
19.
Vacchi-Suzzi C., Kruse D., Harrington J., Levine K., Meliker J.R. Is urinary cadmium a biomarker of long-term exposure in humans? A review. Curr. Environ. Health Rep. 2016; 3(4): 450–458, doi: 10.1007/s40572-016-0107-y.
20.
Wang M., Chen Z., Song W., Hong D., Huang L., Li Y. A review on cadmium exposure in the population and intervention strategies against cadmium toxicity. Bull. Environ. Contam. Toxicol. 2021; 106(1): 65–74, doi: 10.1007/s00128-020-03088-1.
21.
Buha A., Matovic V., Antonijevic B., Bulat Z., Curcic M., Renieri E.A. et al. Overview of cadmium thyroid disrupting effects and mechanisms. Int. J. Mol. Sci. 2018; 19(5): 1501, doi: 10.3390/ijms19051501.
22.
Chandravanshi L., Shiv K., Kumar S. Developmental toxicity of cadmium in infants and children: a review. Environ. Anal. Health Toxicol. 2021; 36(1): e2021003-0, doi: 10.5620/eaht.2021003.
23.
Chunhabundit R. Cadmium exposure and potential health risk from foods in contaminated area, Thailand. Toxicol. Res. 2016; 32(1): 65–72, doi: 10.5487/TR.2016.32.1.065.
24.
Safhi M.M., Khuwaja G., Alam M.F., Hussain S., Siddiqui M.H.A., Islam F. et al. Cadmium-induced nephrotoxicity via oxidative stress in male Wistar rats and capsaicin protects its toxicity. Bull. Env. Pharmacol. Life Sci. 2016; 5(3): 5–11.
25.
Fatima G., Raza A.M., Hadi N., Nigam N., Mahdi A.A. Cadmium in human diseases: It’s more than just a mere metal. Indian J. Clin. Biochem. 2019; 34(4): 371–378, doi: 10.1007/s12291-019-00839-8.
26.
10 chemicals of public health concern. WHO – World Health Organization, 1 June 2020 [online] https://www.who.int/news-room/... [accessed on 6 April 2023].
27.
Shen C., Zhang K., Yang J., Shi J., Yang C., Sun Y. et al. Association between metal(loid)s in serum and leukemia: a systematic review and meta-analysis. J. Environ. Health Sci. Eng. 2023; 21(1): 201–213, doi: 10.1007/s40201-023-00853-2.
28.
Basu N., Bastiansz A., Dórea J.G., Fujimura M., Horvat M., Shroff E. et al. Our evolved understanding of the human health risks of mercury. Ambio 2023; 52(5): 877–896, doi: 10.1007/s13280-023-01831-6.
29.
Barone G., Storelli A., Meleleo D., Dambrosio A., Garofalo R., Busco A. et al. Levels of mercury, methylmercury and selenium in fish: Insights into children food safety. Toxics 2021; 9(2): 39, doi: 10.3390/toxics9020039.
30.
Piekut A., Moskalenko O., Gut K. Can primary teeth be an indicator of the environmental exposure of children to heavy metals? Med. Srod. 2018; 21(4): 18–23, doi: 0.19243/2018402.
31.
Sly P., Blake T., Islam Z. Impact of prenatal and early life environmental exposures on normal human development. Paediatr. Respir. Rev. 2021; 40: 10–14, doi: 10.1016/j.prrv.2021.05.007.
32.
Cao S., Chen X., Zhang L., Xing X., Wen D., Wang B. et al. Quantificational exposure, sources, and health risks posed by heavy metals in indoor and outdoor household dust in a typical smelting area in China. Indoor Air 2020; 30(5): 872–884, doi: 10.1111/ina.12683.
33.
Etzel R.A. The special vulnerability of children. Int. J. Hyg. Environ. Health 2020; 227: 113516, doi: 10.1016/j.ijheh.2020.113516.
34.
Wu H., Xu C., Wang J., Xiang Y., Ren M., Qie H. et al. Health risk assessment based on source identification of heavy metals: A case study of Beiyun River, China. Ecotoxicol. Environ. Saf. 2021; 213: 112046, doi: 10.1016/j.ecoenv.2021.112046.
35.
Esdaile L.J., Chalker J.M. The mercury problem in artisanal and small-scale gold mining. Chemistry 2018; 24(27): 6905–6916, doi: 10.1002/chem.201704840.
36.
Alidadi H., Tavakoly Sany S.B., Zarif Garaati Oftadeh B., Mohamad T., Shamszade H., Fakhari M. Health risk assessments of arsenic and toxic heavy metal exposure in drinking water in northeast Iran. Environ. Health Prev. Med. 2019; 24(1): 59, doi: 10.1186/s12199-019-0812-x.
37.
Piekut A., Gut K., Ćwieląg-Drabek M., Domagalska J., Marchwińska-Wyrwał E. The relationship between children‘s non-nutrient exposure to cadmium, lead and zinc and the location of recreational areas – Based on the Upper Silesia region case (Poland). Chemosphere 2019; 223: 544–550, doi: 10.1016/j.chemosphere.2019.02.085.
38.
Kamińska E. Safety of pharmacotherapy in children in the context of developmental differences. Pediatr. Med. Rodz. 2016; 12(4): 363–374, doi: 10.15557/PiMR.2016.0036.
39.
WHO’s Urban Ambient Air Pollution database – Update 2016. WHO – World Health Organization [online] https://www.who.int/data/gho/d... [accessed on 25 May 2023].
40.
Inheriting a sustainable world: Atlas on children’s health and the environment. WHO – World Health Organization, 6 November 2017 [online] https://www.who.int/publicatio... [accessed on 25 May 2023].
41.
Rozporządzenie Ministra Środowiska z dnia 1 września 2016 r. w sprawie sposobu prowadzenia oceny zanieczyszczenia powierzchni ziemi (Dz.U. 2016 poz. 1395).
42.
Gut K., Rogala D., Marchwińska-Wyrwał E. Exposure to cadmium among consumers of root vegetables cultivated in contaminated soils in Upper Silesia, Poland. Med. Og. Nauk Zdr. 2017; 23(4): 245–249, doi: 10.26444/monz/80448.
43.
A third of the world’s children poisoned by lead, new groundbreaking analysis says. UNICEF.org, 29 July 2020 [online] https://www.unicef.org/press-r... [accessed on 27 October 2023].
44.
Chen H., Chai M., Cheng J., Wang Y., Tang Z. Occurrence and health implications of heavy metals in preschool children’s clothing manufactured in four Asian regions. Ecotoxicol. Environ. Saf. 2022; 245: 114121, doi: 10.1016/j.ecoenv.2022.114121.
45.
Zwolak A., Sarzyńska M., Szpyrka E., Stawarczyk K. Sources of soil pollution by heavy metals and their accumulation in vegetables: a review. Water Air Soil Pollut. 2019; 230(7): 164, doi: 10.1007/s11270-019-4221-y.
46.
Liang G., Gong W., Li B., Zuo J., Pan L., Liu X. Analysis of heavy metals in foodstuffs and an assessment of the health risks to the general public via consumption in Beijing, China. Int. J. Environ. Res. Public Health 2019; 16(6): 909, doi: 10.3390/ijerph16060909.
47.
Yee A.Z., Lwin M.O., Ho S.S. The influence of parental practices on child promotive and preventive food consumption behaviors: a systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017; 14(1): 47, doi: 10.1186/s12966-017-0501-3.
48.
Shim S.M., Lee K. Parents’ knowledge, behaviour and concerns of food chemical hazards: Korean mothers sending their preschool-aged children to child care centres. Int. J. Consumer Stud. 2013; 37(3): 243–249, doi: 10.1111/j.1470-6431.2012.01128.x.
49.
Augustsson A., Lundgren M., Qvarforth A., Hough R., Engström E., Paulukat C. et al. Managing health risks in urban agriculture: The effect of vegetable washing for reducing exposure to metal contaminants. Sci. Total Environ. 2023; 863: 160996, doi: 10.1016/j.scitotenv.2022.160996.
50.
Szefczyk-Polowczyk L., Respondek M. Parents’ education and awareness of the environmental health hazards for children. [Article in Polish]. Med. Srod. 2015; 18(2): 63–64.
51.
Paulson J.A., Arnesen S.J. The use of the Internet for children’s health and the environment. Pediatr. Clin. North Am. 2007; 54(1): 135–153, doi: 10.1016/j.pcl.2006.11.011.
Share
RELATED ARTICLE
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.