Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
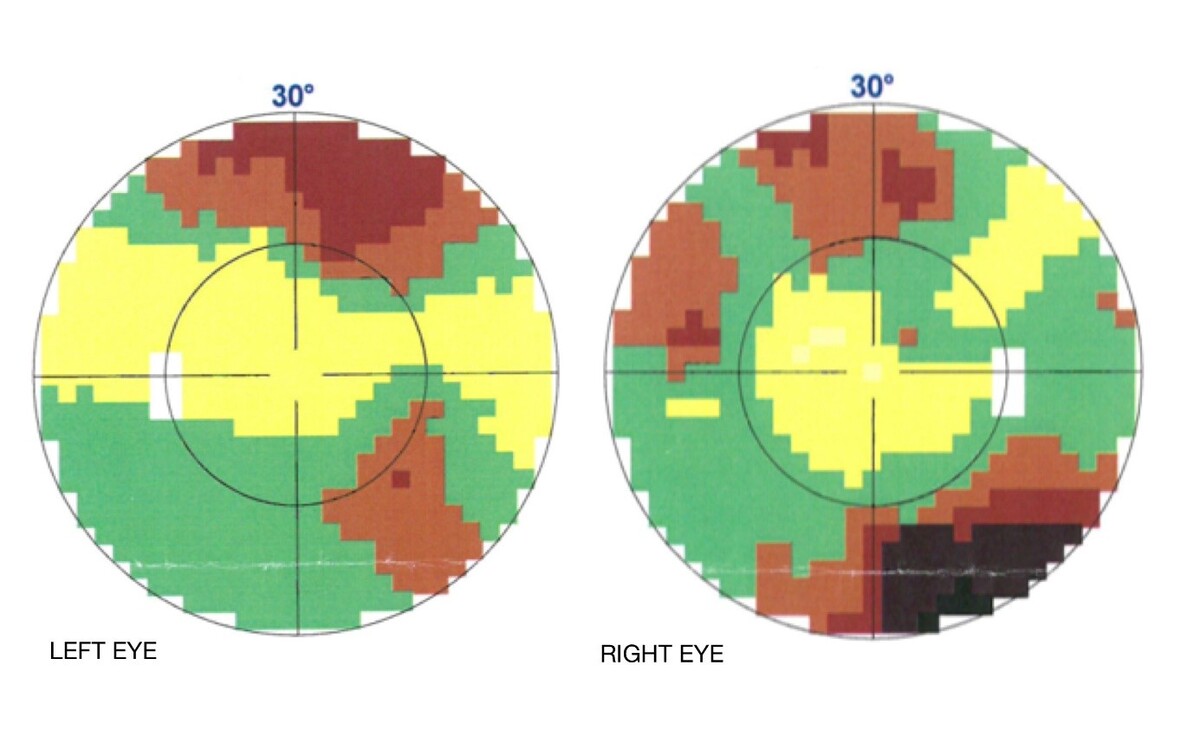
Visual field defects in the course of bipolar affective disorder in a teenager
1
Department of Ophthalmology, Independent Public Health Care Center No. 1 in Rzeszów, Poland
2
Świętokrzyskie Centrum Reumatologii, Zespół Opieki Zdrowotnej w Końskich
3
Oddział Chorób Wewnętrznych, Endokrynologii, Diabetologii i Gastroenterologii, Szpital Wojewódzki w Opolu
4
Department of Endocrinology and Diabetology, Antoni Jurasz University Hospital No. 1 in Bydgoszcz, Poland
5
Department of Paediatrics Ophthalmology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
Corresponding author
Aleksandra Ziemba
Oddział Okulistyki, Samodzielny Publiczny Zespół Opieki Zdrowotnej Nr 1 w Rzeszowie, ul. Rycerska 4, 35-241 Rzeszów
Oddział Okulistyki, Samodzielny Publiczny Zespół Opieki Zdrowotnej Nr 1 w Rzeszowie, ul. Rycerska 4, 35-241 Rzeszów
Ann. Acad. Med. Siles. 2025;79:355-360
KEYWORDS
TOPICS
ABSTRACT
Visual field defects are associated with diseases of visual and central nervous systems or pituitary gland, such as retinopathies, optic nerve disorders and visual pathway pathologies or proliferative conditions. A 17-year-old girl with multiple endocrine illnesses – hyperprolactinemia, hypothyroidism, hyperinsulinemia, obesity and bipolar affective disorder – reported visual field disturbances, which were confirmed in kinetic and static visual field examination. Magnetic resonance imaging of the head did not reveal any significant pathologies. Fundus examination showed no abnormalities. The severity of visual field defects changed over time. There were periods of deterioration, when the field of vision narrowed into a tunnel vision, and periods of improvement. A thorough history taking and analysis of psychiatric documentation indicated that episodes of visual field disturbances depended on the phase of bipolar disorder. During mania, the field of vision improved, and during depression, it worsened. This case report shows that not only somatic diseases can lead to visual field defects. After excluding proliferative conditions, central nervous systems or retinal degeneration, it is necessary to expand the differential diagnosis to include a thorough medical history including psychiatric diseases in the family, as well as a psychiatric examination of the patient. The exclusion of optic neuropathy and structural brain changes in the presented patient suggest that the symptoms are caused by bipolar affective disorder.
REFERENCES (22)
1.
Grande I., Berk M., Birmaher B., Vieta E. Bipolar disorder. Lancet 2016; 387(10027): 1561–1572, doi: 10.1016/S0140-6736(15)00241-X.
2.
Broniarczyk-Czarniak M.J., Sowińska K., Białas J., Talarowska M. Ciężka depresja z nasilonymi zaburzeniami funkcji poznawczych czy otępienie? Psychiatria 2019; 16(4): 218–226.
3.
Carvalho A.F., Firth J., Vieta E. Bipolar disorder. N. Engl. J. Med. 2020; 383(1): 58–66, doi: 10.1056/NEJMra1906193 .
4.
Gałecki P., Szulc A. Zaburzenia nastroju (afektywne) (F30-F39). In: Psychiatria. Edra Urban & Partner. Wrocław 2020, s. 189–235.
5.
Liou Y.J., Chen M.H., Hsu J.W., Huang K.L., Huang P.H., Bai Y.M. Levels of circulating endothelial progenitor cells inversely correlate with manic and positive symptom severity in patients with bipolar disorder. Brain Behav. 2022; 12(6): e2570, doi: 10.1002/brb3.2570.
6.
Brunner R., Jägle H., Kandsperger S. Dissociative visual loss in children and adolescents. Klin. Monbl. Augenheilkd. 2021; 238(10): 1084–1091, doi: 10.1055/a-1617-3193.
7.
Somers A., Casteels K., Van Roie E., Spileers W., Casteels I. Non-organic visual loss in children: prospective and retrospective analysis of associated psychosocial problems and stress factors. Acta Ophthalmol. 2016; 94(5): e312–e326, doi: 10.1111/aos.12848.
8.
Moore Q., Al-Zubidi N., Yalamanchili S., Lee A.G. Nonorganic visual loss in children. Int. Ophthalmol. Clin. 2012; 52(3): 107–123, xii, doi: 10.1097/IIO.0b013e31825a1201.
9.
Mojon D.S., Schläpfer T.E. Nonorganic disorders in ophthalmology: overview of diagnosis and therapy. [Article in German]. Klin. Monbl. Augenheilkd. 2001; 218(5): 298–304, doi: 10.1055/s-2001-15885.
10.
Vieta E., Salagre E., Grande I., Carvalho A.F., Fernandes B.S., Berk M. et al. Early intervention in bipolar disorder. Am. J. Psychiatry 2018; 175(5): 411–426, doi: 10.1176/appi.ajp.2017.17090972.
11.
Cichoń L., Janas-Kozik M., Siwiec A., Rybakowski J.K. Clinical picture and treatment of bipolar affective disorder in children and adolescents. Psychiatr. Pol. 2020; 54(1): 35–50, doi: 10.12740/PP/OnlineFirst/92740.
12.
Birmaher B., Axelson D., Strober M., Gill M.K., Yang M., Ryan N. et al. Comparison of manic and depressive symptoms between children and adolescents with bipolar spectrum disorders. Bipolar Disord. 2009; 11(1): 52–62, doi: 10.1111/j.1399-5618.2008.00659.x.
13.
Fernandes T.M.P., Andrade S.M., de Andrade M.J.O., Nogueira R.M.T.B.L., Santos N.A. Colour discrimination thresholds in type 1 Bipolar Disorder: a pilot study. Sci. Rep. 2017; 7(1): 16405, doi: 10.1038/s41598-017-16752-0.
14.
Zheng W., Tang L.R., Correll C.U., Ungvari G.S., Chiu H.F., Xiang Y.Q. et.al. Frequency and correlates of distant visual impairment in patients with schizophrenia, bipolar disorder, and major depressive disorder. East Asian Arch. Psychiatry 2015; 25(3): 115–121.
15.
Fernandes T.P., Shoshina I.I., Oliveira M.E.C., Andreevna V.E., Silva G.M., Santos N.A. Correlates of clinical variables on early-stage visual processing in schizophrenia and bipolar disorder. J. Psychiatr. Res. 2022; 149: 323–330, doi: 10.1016/j.jpsychires.2022.03.014.
16.
Garcia-Martin E., Gavin A., Garcia-Campayo J., Vilades E., Orduna E., Polo V. et al. Visual function and retinal changes in patients with bipolar disorder. Retina 2019; 39(10): 2012–2021, doi: 10.1097/IAE.0000000000002252.
17.
Satue M., Fuentes J.L., Vilades E., Orduna E., Vicente M.J., Cordon B. et al. Evaluation of progressive retinal degeneration in bipolar disorder patients over a period of 5 years. Curr. Eye Res. 2022; 47(7): 1061–1067, doi: 10.1080/02713683.2022.2064513.
18.
Vilades Palomar E., Cipres M., Obis J., Rodrigo M.J., Satue M., Garcia-Martin E. Changes in visual function and retinal structure in patients with manic-depressive illness or bipolar disorder. Acta Ophthalmol. 2017; 95(S259), doi: 10.1111/j.1755-3768.2017.0T024.
19.
Jung K.I., Hong S.Y., Shin D.Y., Lee N.Y., Kim T.S., Park C.K. Attenuated visual function in patients with major depressive disorder. J. Clin. Med. 2020; 9(6): 1951, doi: 10.3390/jcm9061951.
20.
Li J., Tripathi R.C., Tripathi B.J. Drug-induced ocular disorders. Drug Saf. 2008; 31(2): 127–141, doi: 10.2165/00002018-200831020-00003.
21.
Pesando P., Nuzzi G., Maraini G. Bilateral papilloedema in long term therapy with lithium carbonate. Pharmakopsychiatr. Neuropsychopharmakol. 1980; 13(4): 235–239, doi: 10.1055/s-2007-1019636.
22.
Kaufman P.L., Jefferson J.W., Ackerman D., Baumgartner S. Ocular effects of oral lithium in humans. Acta Ophthalmol. 1985; 63(3): 327–332, doi: 10.1111/j.1755-3768.1985.tb06815.x.
Share
RELATED ARTICLE
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.