Current issue
About the Journal
Scientific Council
Editorial Board
Regulatory and archival policy
Code of publishing ethics
Publisher
Information about the processing of personal data in relation to cookies and newsletter subscription
Archive
For Authors
For Reviewers
Contact
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
Links
Sklep Wydawnictwa SUM
Biblioteka Główna SUM
Śląski Uniwersytet Medyczny w Katowicach
Privacy policy
Accessibility statement
Reviewers
Annals reviewers in 2025
Annals reviewers in 2024
Annals reviewers in 2023
Annals reviewers in 2022
Annals reviewers in 2021
Annals reviewers in 2020
Annals reviewers in 2019
Annals reviewers in 2018
Annals reviewers in 2017
Annals reviewers in 2016
Annals reviewers in 2015
Annals reviewers in 2014
Annals reviewers in 2013
Annals reviewers in 2012
A quality of body posture in early school-aged children after a pandemic and selected lifestyle components – preliminary report
1
Department of Physiotherapy, Faculty of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland
2
Doctoral School, Medical University of Silesia, Katowice, Poland
Corresponding author
Anna Brzęk
Zakład Fizjoterapii, Wydział Nauk o Zdrowiu w Katowicach, Śląski Uniwersytet Medyczny w Katowicach, ul. Medyków 12
Zakład Fizjoterapii, Wydział Nauk o Zdrowiu w Katowicach, Śląski Uniwersytet Medyczny w Katowicach, ul. Medyków 12
Ann. Acad. Med. Siles. 2024;1(nr specj.):27-34
KEYWORDS
TOPICS
ABSTRACT
Introduction:
There are many modifiable risk factors that disrupt proper motor development, including the development of body posture. Abnormal body positions taken repeatedly, frequent use of electronic devices, and motor passivity are all implicated in postural abnormalities. In the post-pandemic period, sedentary behavior is quite common among children and adolescents, contributing to increased overweight and obesity, as well as changes in lifestyle, which consequently lead to many health problems. The main aim of this study was to assess the quality of children’s body posture and attempt to estimate the relationship between the occurrence of postural abnormalities and the level of physical activity.
Material and methods:
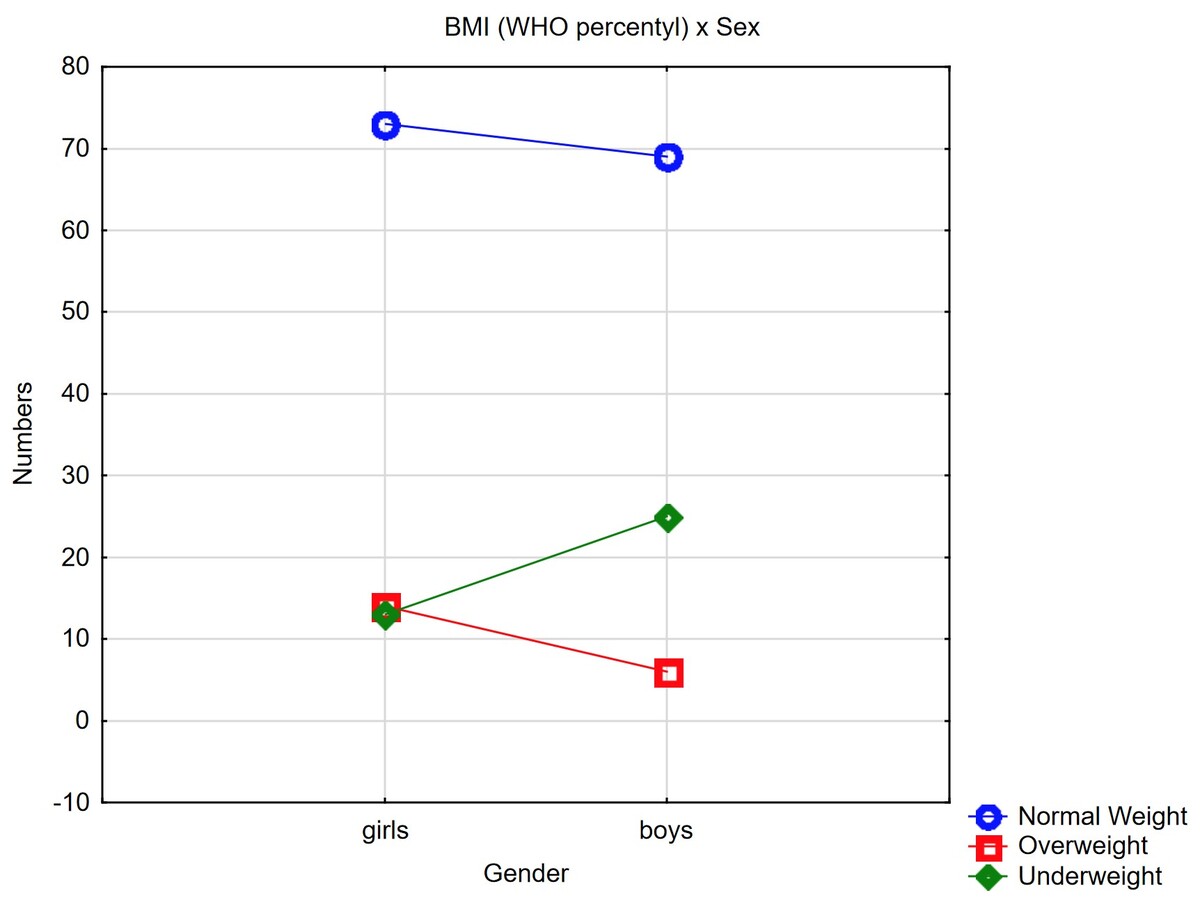
A pilot study was conducted on a sample of 200 children from early elementary school classes in the Silesia region, aged 6–10 years (x = 8.25 ± 1.06). The respondents were classified into two subgroups of equal size of 100 girls (group I) and 100 boys (group II). The study groups did not have any differences in age (p = 0.07). Body posture was assessed in all three planes using a plumb line, scoliometer, and inclinometer, as well as functional status with Thomayer and Matthias tests. Body weight and height were measured using a Tanita analyzer and stadiometer with conversion to centile charts for weight, height, and body mass index (BMI).
Results:
Postural defects in the sagittal plane in both the thoracic and lumbar segments were found in approximately 20% of the subjects in both groups, regardless of the level of physical activity. In both study groups, excessive screen time and time spent in a sitting position were observed. Physical activity was largely below World Health Organization (WHO) recommendations.
Conclusions:
Children of younger school age are noted to have numerous postural abnormalities that are unrelated to their level of physical activity. Children use screen time and spend too much time sitting and do not meet WHO recommendations for moderate to vigorous physical activity.
There are many modifiable risk factors that disrupt proper motor development, including the development of body posture. Abnormal body positions taken repeatedly, frequent use of electronic devices, and motor passivity are all implicated in postural abnormalities. In the post-pandemic period, sedentary behavior is quite common among children and adolescents, contributing to increased overweight and obesity, as well as changes in lifestyle, which consequently lead to many health problems. The main aim of this study was to assess the quality of children’s body posture and attempt to estimate the relationship between the occurrence of postural abnormalities and the level of physical activity.
Material and methods:
A pilot study was conducted on a sample of 200 children from early elementary school classes in the Silesia region, aged 6–10 years (x = 8.25 ± 1.06). The respondents were classified into two subgroups of equal size of 100 girls (group I) and 100 boys (group II). The study groups did not have any differences in age (p = 0.07). Body posture was assessed in all three planes using a plumb line, scoliometer, and inclinometer, as well as functional status with Thomayer and Matthias tests. Body weight and height were measured using a Tanita analyzer and stadiometer with conversion to centile charts for weight, height, and body mass index (BMI).
Results:
Postural defects in the sagittal plane in both the thoracic and lumbar segments were found in approximately 20% of the subjects in both groups, regardless of the level of physical activity. In both study groups, excessive screen time and time spent in a sitting position were observed. Physical activity was largely below World Health Organization (WHO) recommendations.
Conclusions:
Children of younger school age are noted to have numerous postural abnormalities that are unrelated to their level of physical activity. Children use screen time and spend too much time sitting and do not meet WHO recommendations for moderate to vigorous physical activity.
ACKNOWLEDGEMENTS
The Authors thank all children and their parents who participated in this investigations.
FUNDING
Co-financed by the “Social Responsibility of Science” program of the Ministry of Education and Science (2023–2024).
CONFLICT OF INTEREST
Non-declared.
REFERENCES (27)
1.
Nowotny J. Ćwiczenia korekcyjne w systemie stacyjnym. Wyd. Akademii Wychowania Fizycznego w Katowicach. Katowice 2001.
2.
Kasperczyk T. Wady postawy ciała – diagnostyka i leczenie. Wyd. Kasper. Kraków 1998.
3.
Brzęk A., Plinta R. Exemplification of movement patterns and their influence on body posture in younger school-age children on the basis of an authorial program “I take care of my spine”. Medicine (Baltimore) 2016; 95(12): e2855, doi: 10.1097/MD.0000000000002855.
4.
Kędra A., Plandowska M., Kędra P., Czaprowski D. Non-specific low back pain: cross-sectional study of 11,423 children and youth and the association with the perception of heaviness in carrying of schoolbags. PeerJ 2021; 9: e11220, doi: 10.7717/peerj.11220.
5.
Brzęk A., Kozinoga M., Stoliński Ł. Fizjoprofilaktyka skolioz niskostopniowych. In: M. Grygorowicz, M. Podhorecka [ed.]. Kompendium fizjoprofilaktyki. Wyd. Nauk. Uniwersytetu Medycznego im. Karola Marcinkowskiego w Poznaniu. Poznań 2020, p. 149–158.
6.
Czaprowski D., Woźniak-Kasperek E., Wiernicka M. Fizjoprofilaktyka zaburzeń postawy ciała. In: M. Grygorowicz, M. Podhorecka [ed.]. Kompendium fizjoprofilaktyki. Wyd. Nauk. Uniwersytetu Medycznego im. Karola Marcinkowskiego w Poznaniu. Poznań 2020, p. 137–146.
7.
Czaprowski D., Gwiazdowska-Czubak K., Tyrakowski M., Kędra A. Sagittal body alignment in a sitting position in children is not affected by the generalized joint hypermobility. Sci. Rep. 2021; 11(1): 13748, doi: 10.1038/s41598-021-93215-7.
8.
Chaput J.P., Willumsen J., Bull F., Chou R., Ekelund U., Firth J. et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 2020; 26; 17(1): 141, doi: 10.1186/s12966-020-01037-z.
9.
Get moving: Key takeaways from the new physical activity guidelines. NIH MedlinePlus Magazine, April 04, 2019 [online] https://magazine.medlineplus.g... [accessed on 4 April 2024].
10.
Willumsen J., Bull F. Development of WHO guidelines on physical activity, sedentary behavior, and sleep for children less than 5 years of age. J. Phys. Act. Health 2020; 17(1): 96–100, doi: 10.1123/jpah.2019-0457.
11.
World Health Organization. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age: web annex: evidence profiles. World Health Organization, https://apps.who.int/iris/hand.... License: CC BY-NC-SA 3.0 IGO.
12.
Brzęk A., Strauss M., Przybylek B., Dworrak T., Dworrak B., Leischik R. How does the activity level of the parents influence their children’s activity? The contemporary life in a world ruled by electronic devices. Arch. Med. Sci. 2018; 14(1): 190–198, doi: 10.5114/aoms.2018.72242.
13.
Langøy A., Smith O.R.F., Wold B., Samdal O., Haug E.M. Associations between family structure and young people’s physical activity and screen time behaviors. BMC Public Health 2019; 19(1): 433, doi: 10.1186/s12889-019-6740-2.
14.
Zakrzewski-Fruer J.K., Gillison F.B., Katzmarzyk P.T., Mire E.F., Broyles S.T., Champagne C.M. et al. Association between breakfast frequency and physical activity and sedentary time: a cross-sectional study in children from 12 countries. BMC Public Health 2019; 19(1): 222, doi: 10.1186/s12889-019-6542-6.
15.
Salway R., de Vocht F., Emm-Collison L., Sansum K., House D., Walker R. et al. Comparison of children’s physical activity profiles before and after COVID-19 lockdowns: A latent profile analysis. PLoS One 2023; 18(11): e0289344, doi: 10.1371/journal.pone.0289344.
16.
Jago R., Salway R., House D., Walker R., Emm-Collison L., Sansum K. et al. Short and medium-term effects of the COVID-19 lockdowns on child and parent accelerometer-measured physical activity and sedentary time: a natural experiment. Int. J. Behav. Nutr. Phys. Act. 2023; 20(1): 42, doi: 10.1186/s12966-023-01441-1.
17.
Skrede T., Steene‐Johannessen J., Anderssen S.A., Resaland G.K., Ekelund U. The prospective association between objectively measured sedentary time, moderate‐to‐vigorous physical activity and cardiometabolic risk factors in youth: a systematic review and meta‐analysis. Obes. Rev. 2019; 20(1): 55–74, doi: 10.1111/obr.12758.
18.
Currie C., Morgan A. A bio-ecological framing of evidence on the determinants of adolescent mental health – A scoping review of the interna-tional Health Behaviour in School-Aged Children (HBSC) study 1983–2020. SSM Popul. Health 2020; 12: 100697, doi: 10.1016/j.ssmph.2020.100697.
19.
Czaprowski D., Stoliński Ł., Szczygieł A., Kędra A. Sedentary behaviours of girls and boys aged 7–15. Pol. J. Public Health 2011; 121(3): 248–252.
20.
Brzęk A., Strauss M., Sanchis-Gomar F., Leischik R. Physical activity, screen time, sedentary and sleeping habits of Polish preschoolers during the COVID-19 pandemic and WHO’s recommendations: an observational cohort study. Int. J. Environ. Res. Public Health 2021; 18(21): 11173.
21.
Aguilar-Cordero M.J., León Ríos X.A., Rojas-Carvajal A.M., Latorre-García J., Expósito-Ruiz M., Sánchez-López A.M. Effects of physical activity on quality of life in overweight and obese children. Nutr. Hosp. 2021; 38(4): 736–741, doi: 10.20960/nh.03373.
22.
Pearce A., Hope S., Griffiths L., Cortina-Borja M., Chittleborough C., Law C. What if all children achieved WHO recommendations on physical activity? Estimating the impact on socioeconomic inequalities in childhood overweight in the UK Millennium Cohort Study. Int. J. Epidemiol. 2019; 48(1): 134–147, doi: 10.1093/ije/dyy267.
23.
Rodriguez-Ayllon M., Cadenas-Sánchez C., Estévez-López F., Munoz N.E., Mora-Gonzalez J., Migueles J.H. et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 2019; 49(9): 1383–1410, doi: 10.1007/s40279-019-01099-5.
24.
Sherar L.B., Griffin T.P., Ekelund U., Cooper A.R., Esliger D.W., van Sluijs E.M.F. et al. Association between maternal education and objectively measured physical activity and sedentary time in adolescents. J. Epidemiol. Community Health 2016; 70(6): 541–548, doi: 10.1136/jech-2015-205763.
25.
Xie G., Deng Q., Cao J., Chang Q. Digital screen time and its effect on preschoolers’ behavior in China: results from a cross-sectional study. Ital. J. Pediatr. 2020; 46(1): 9, doi: 10.1186/s13052-020-0776-x.
26.
Schwarzfischer P., Gruszfeld D., Socha P., Luque V., Closa-Monasterolo R., Rousseaux D. et al. Effects of screen time and playing outside on anthropometric measures in preschool aged children. PLoS One 2020; 15(3): e0229708, doi: 10.1371/journal.pone.0229708.
27.
De Decker E., De Craemer M., De Bourdeaudhuij I., Wijndaele K., Duvinage K., Koletzko B. et al. Influencing factors of screen time in preschool children: an exploration of parents’ perceptions through focus groups in six European countries. Obes. Rev. 2012; 13(Suppl 1): 75–84, doi: 10.1111/j.1467-789X.2011.00961.x.
CITATIONS (2):
1.
Children with abnormal body weight dealing with the load of school backpack—is there a need to modify WHO recommendations? A cross sectional study
Anna Brzęk, Regina Wysocka-Bochenek, Jacek Sołtys
PeerJ
Anna Brzęk, Regina Wysocka-Bochenek, Jacek Sołtys
PeerJ
2.
The school backpack and physical parameters relationship with spinal alignment in the sagittal plane. Are changes in the design of school backpacks for younger school-age children necessary?
Anna Brzęk, Regina Wysocka-Bochenek, Jacek Sołtys, Agata Chmielarz
Polish Journal of Medical Physics and Engineering
Anna Brzęk, Regina Wysocka-Bochenek, Jacek Sołtys, Agata Chmielarz
Polish Journal of Medical Physics and Engineering
Share
RELATED ARTICLE
The Medical University of Silesia in Katowice, as the Operator of the annales.sum.edu.pl website, processes personal data collected when visiting the website. The function of obtaining information about Users and their behavior is carried out by voluntarily entered information in forms, saving cookies in end devices, as well as by collecting web server logs, which are in the possession of the website Operator. Data, including cookies, are used to provide services in accordance with the Privacy policy.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.
You can consent to the processing of data for these purposes, refuse consent or access more detailed information.