Bieżący numer
O czasopiśmie
Rada Naukowa
Kolegium Redakcyjne
Polityka prawno-archiwizacyjna
Kodeks etyki publikacyjnej
Wydawca
Informacja o przetwarzaniu danych osobowych w ramach plików cookies oraz subskrypcji newslettera
Archiwum
Dla autorów
Dla recenzentów
Kontakt
Recenzenci
Recenzenci rocznika 2025
Recenzenci rocznika 2024
Recenzenci rocznika 2023
Recenzenci rocznika 2022
Recenzenci rocznika 2021
Recenzenci rocznika 2020
Recenzenci rocznika 2019
Recenzenci rocznika 2018
Recenzenci rocznika 2017
Recenzenci rocznika 2016
Recenzenci rocznika 2015
Recenzenci rocznika 2014
Recenzenci rocznika 2013
Recenzenci rocznika 2012
Polecamy
Śląski Uniwersytet Medyczny w Katowicach
Sklep Wydawnictw SUM
Biblioteka Główna SUM
Polityka prywatności
Deklaracja dostępności
Recenzenci
Recenzenci rocznika 2025
Recenzenci rocznika 2024
Recenzenci rocznika 2023
Recenzenci rocznika 2022
Recenzenci rocznika 2021
Recenzenci rocznika 2020
Recenzenci rocznika 2019
Recenzenci rocznika 2018
Recenzenci rocznika 2017
Recenzenci rocznika 2016
Recenzenci rocznika 2015
Recenzenci rocznika 2014
Recenzenci rocznika 2013
Recenzenci rocznika 2012
Czy pandemia COVID-19 ma wpływ na poczucie strachu i obawy u kobiet będących w ciąży?
1
Students’ Scientific Club, Department of Gynaecology and Obstetrics, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
2
Department of Gynaecology and Obstetrics, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
Autor do korespondencji
Mateusz Zabochnicki
Katedra i Klinika Ginekologii i Położnictwa, Śląski Uniwersytet Medyczny w Katowicach, ul. Medyków 14, 40-752 Katowice
Katedra i Klinika Ginekologii i Położnictwa, Śląski Uniwersytet Medyczny w Katowicach, ul. Medyków 14, 40-752 Katowice
Ann. Acad. Med. Siles. 2024;78:309-316
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie:
Objawy lękowe i depresyjne są powszechnymi objawami w okresie ciąży. Wystąpienie pandemii wirusa COVID-19 jest wyjątkowym stresorem, który wpłynął na psychologiczny aspekt przebiegu porodu. Celem pracy jest ocena wpływu pandemii COVID-19 na przebieg ciąży i porodu w populacji polskiej.
Materiał i metody:
Grupę badawczą stanowiło 2186 kobiet. Badanie ankietowe zostało przeprowadzone w okresie od listopada 2020 r. do grudnia 2020 r. za pośrednictwem Internetu. Kryterium włączenia do badania były ciąża i poród w okresie pandemii COVID-19. Do oceny stopnia poziomu strachu i obaw wykorzystano pytania stworzone przez autorów z zastosowaniem pięciostopniowej skali Likerta.
Wyniki:
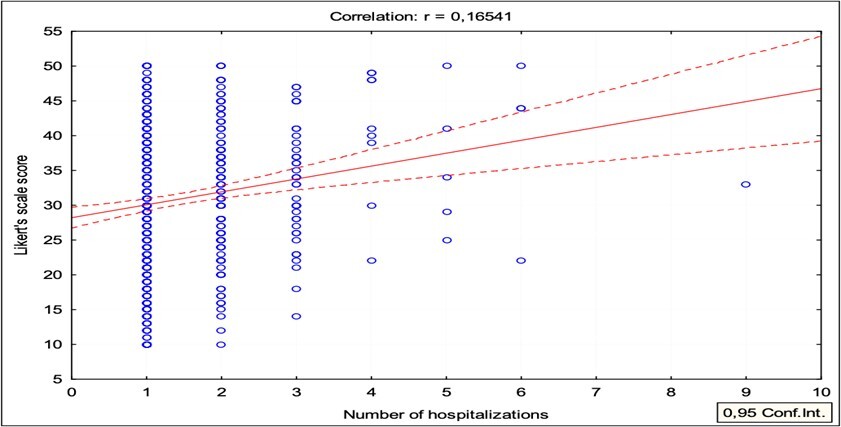
U kobiet hospitalizowanych w czasie ciąży występował większy poziom strachu i obaw związanych z ciążą (średnia 30,9 vs 29,6; p = 0,007). Podobną zależność stwierdzono w przypadku kobiet, u których wykonano cesarskie cięcie (30,6 vs 29,5; p = 0,006) lub które były hospitalizowane > 7 dni (31,8 vs 29,7; p = 0,012). Stwierdzono również istotną statystycznie, choć słabą korelację pomiędzy średnimi wynikami pytań dotyczących obaw a liczbą hospitalizacji w czasie ciąży (współczynnik korelacji Pearsona r = 0,1654; p < 0,000).
Wnioski:
Badanie wykazało alarmująco wysoki poziom lęku u kobiet w ciąży podczas pandemii COVID-19, co może mieć długoterminowe konsekwencje dla ich dzieci.
Objawy lękowe i depresyjne są powszechnymi objawami w okresie ciąży. Wystąpienie pandemii wirusa COVID-19 jest wyjątkowym stresorem, który wpłynął na psychologiczny aspekt przebiegu porodu. Celem pracy jest ocena wpływu pandemii COVID-19 na przebieg ciąży i porodu w populacji polskiej.
Materiał i metody:
Grupę badawczą stanowiło 2186 kobiet. Badanie ankietowe zostało przeprowadzone w okresie od listopada 2020 r. do grudnia 2020 r. za pośrednictwem Internetu. Kryterium włączenia do badania były ciąża i poród w okresie pandemii COVID-19. Do oceny stopnia poziomu strachu i obaw wykorzystano pytania stworzone przez autorów z zastosowaniem pięciostopniowej skali Likerta.
Wyniki:
U kobiet hospitalizowanych w czasie ciąży występował większy poziom strachu i obaw związanych z ciążą (średnia 30,9 vs 29,6; p = 0,007). Podobną zależność stwierdzono w przypadku kobiet, u których wykonano cesarskie cięcie (30,6 vs 29,5; p = 0,006) lub które były hospitalizowane > 7 dni (31,8 vs 29,7; p = 0,012). Stwierdzono również istotną statystycznie, choć słabą korelację pomiędzy średnimi wynikami pytań dotyczących obaw a liczbą hospitalizacji w czasie ciąży (współczynnik korelacji Pearsona r = 0,1654; p < 0,000).
Wnioski:
Badanie wykazało alarmująco wysoki poziom lęku u kobiet w ciąży podczas pandemii COVID-19, co może mieć długoterminowe konsekwencje dla ich dzieci.
REFERENCJE (55)
1.
WHO Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020. World Health Organization, 11 March 2020 [online] https://www.who.int/dg/speeche... [accessed on 30 April 2022].
2.
Makowska M., Boguszewski R., Nowakowski M., Podkowińska M. Self-medication-related behaviors and Poland’s COVID-19 lockdown. Int. J. Environ. Res. Public Health 2020; 17(22): 8344, doi: 10.3390/ijerph17228344.
3.
Jones E.A.K., Mitra A.K., Bhuiyan A.R. Impact of COVID-19 on mental health in adolescents: A systematic review. Int. J. Environ. Res. Public Health 2021; 18(5): 2470, doi: 10.3390/ijerph18052470.
4.
Hossain M.M., Tasnim S., Sultana A., Faizah F., Mazumder H., Zou L. et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020; 9: 636, doi: 10.12688/f1000research.24457.1.
5.
Cohen S.D., Cukor D., Kimmel P.L. Anxiety in patients treated with hemodialysis. Clin. J. Am. Soc. Nephrol. 2016; 11(12): 2250–2255, doi: 10.2215/CJN.02590316.
6.
Miralles O., Sanchez-Rodriguez D., Marco E., Annweiler C., Baztan A., Betancor É. et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: a report from six European countries. Eur. Geriatr. Med. 2021; 12(1): 193–204, doi: 10.1007/s41999-020-00415-x.
7.
Şahi̇n D., Tanaçan A., Webster S.N., Moraloğlu Tekin Ö. Pregnancy and COVID-19: prevention, vaccination, therapy, and beyond. Turk. J. Med. Sci. 2021; 51(SI-1): 3312–3326, doi: 10.3906/sag-2106-134.
8.
Kohlhepp L.M., Hollerich G., Vo L., Hofmann-Kiefer K., Rehm M., Louwen F. et al. Physiological changes during pregnancy. [Article in German]. Anaesthesist 2018; 67(5): 383–396, doi: 10.1007/s00101-018-0437-2.
9.
Bjelica A., Cetkovic N., Trninic-Pjevic A., Mladenovic-Segedi L. The phenomenon of pregnancy — a psychological view. Ginekol. Pol. 2018; 89(2): 102–106, doi: 10.5603/GP.a2018.0017.
10.
Salem D., Katranji F., Bakdash T. COVID‐19 infection in pregnant women: Review of maternal and fetal outcomes. Int. J. Gynaecol. Obstet. 2021; 152(3): 291–298, doi: 10.1002/ijgo.13533.
11.
Schwartz D.A. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: Maternal coronavirus infections and pregnancy outcomes. Arch. Pathol. Lab. Med. 2020; 144(7): 799–805, doi: 10.5858/arpa.2020-0901-SA.
12.
Dashraath P., Wong J.L.J., Lim M.X.K., Lim L.M., Li S., Biswas A. et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020; 222(6): 521–531, doi: 10.1016/j.ajog.2020.03.021.
13.
Webster Marketon J.I., Glaser R. Stress hormones and immune function. Cell. Immunol. 2008; 252(1–2): 16–26, doi: 10.1016/j.cellimm.2007.09.006.
14.
Wastnedge E.A.N., Reynolds R.M., van Boeckel S.R., Stock S.J., Denison F.C., Maybin J.A. et al. Pregnancy and COVID-19. Physiol. Rev. 2021; 101(1): 303–318, doi: 10.1152/physrev.00024.2020.
15.
Servante J., Swallow G., Thornton J.G., Myers B., Munireddy S., Malinowski A.K. et al. Haemostatic and thrombo-embolic complications in pregnant women with COVID-19: a systematic review and critical analysis. BMC Pregnancy Childbirth 2021; 21(1): 108, doi: 10.1186/s12884-021-03568-0.
16.
Adeyanju G.C., Engel E., Koch L., Ranzinger T., Shahid I.B.M., Head M.G. et al. Determinants of influenza vaccine hesitancy among pregnant women in Europe: a systematic review. Eur. J. Med. Res. 2021; 26(1): 116, doi: 10.1186/s40001-021-00584-w.
17.
Wang C.L., Liu Y.Y., Wu C.H., Wang C.Y., Wang C.H., Long C.Y. Impact of COVID-19 on pregnancy. Int. J. Med. Sci. 2021; 18(3): 763–767, doi: 10.7150/ijms.49923.
18.
Jamieson D.J., Rasmussen S.A. An update on COVID-19 and pregnancy. Am. J. Obstet. Gynecol. 2022; 226(2): 177–186, doi: 10.1016/j.ajog.2021.08.054.
19.
Mah B.L., Pringle K.G., Weatherall L., Keogh L., Schumacher T., Eades S. et al. Pregnancy stress, healthy pregnancy and birth outcomes – the need for early preventative approaches in pregnant Australian Indigenous women: a prospective longitudinal cohort study. J. Dev. Orig. Health Dis. 2019; 10(1): 31–38, doi: 10.1017/S204017441800079X.
20.
Bayrampour H., Ali E., McNeil D.A., Benzies K., MacQueen G., Tough S. Pregnancy-related anxiety: A concept analysis. Int. J. Nurs. Stud. 2016; 55: 115–130, doi: 10.1016/j.ijnurstu.2015.10.023.
21.
van den Bergh B.R.H., Dahnke R., Mennes M. Prenatal stress and the developing brain: Risks for neurodevelopmental disorders. Dev. Psychopathol. 2018; 30(3): 743–762, doi: 10.1017/S0954579418000342.
22.
Silva M.M.J., Nogueira D.A., Clapis M.J., Leite E.P.R.C. Anxiety in pregnancy: prevalence and associated factors. Rev. Esc. Enferm. USP. 2017; 51: e03253, doi: 10.1590/S1980-220X2016048003253.
23.
Biaggi A., Conroy S., Pawlby S., Pariante C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016; 191: 62–77, doi: 10.1016/j.jad.2015.11.014.
24.
Oliveira C., Imakawa T.D.S., Moisés E.C.D. Physical activity during pregnancy: Recommendations and assessment tools. Rev. Bras. Ginecol. Obstet. 2017; 39(8): 424–432, doi: 10.1055/s-0037-1604180.
25.
Thomas J.C., Letourneau N., Campbell T.S., Giesbrecht G.F. Social buffering of the maternal and infant HPA axes: Mediation and moderation in the intergenerational transmission of adverse childhood experiences. Dev. Psychopathol. 2018; 30(3): 921–939, doi: 10.1017/S0954579418000512.
26.
Naghizadeh S., Mirghafourvand M. Relationship of fear of COVID-19 and pregnancy-related quality of life during the COVID-19 pandemic. Arch. Psychiatr. Nurs. 2021; 35(4): 364–368, doi: 10.1016/j.apnu.2021.05.006.
27.
Almeida M., Shrestha A.D., Stojanac D., Miller L.J. The impact of the COVID-19 pandemic on women’s mental health. Arch. Womens Ment. Health 2020; 23(6): 741–748, doi: 10.1007/s00737-020-01092-2.
28.
Svensson E. Construction of a single global scale for multi-item assessments of the same variable. Stat. Med. 2001; 20(24): 3831–3846, doi: 10.1002/sim.1148.
29.
Dourado G.B., Volpato G.H., de Almeida-Pedrin R.R., Pedron Oltramari P.V., Freire Fernandes T.M., de Castro Ferreira Conti A.C. Likert scale vs visual analog scale for assessing facial pleasantness. Am. J. Orthod. Dentofacial Orthop. 2021; 160(6): 844–852, doi: 10.1016/j.ajodo.2020.05.024.
30.
Rashidi Fakari F., Simbar M. Coronavirus pandemic and worries during pregnancy; a letter to editor. Arch. Acad. Emerg. Med. 2020; 8(1): e21.
31.
Preis H., Mahaffey B., Heiselman C., Lobel M. Pandemic-related pregnancy stress and anxiety among women pregnant during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. MFM 2020; 2(3): 100155, doi: 10.1016/j.ajogmf.2020.100155.
32.
Satici B., Saricali M., Satici S.A., Griffiths M.D. Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Int. J. Ment. Health Addict. 2022; 20(5): 2731–2742, doi: 10.1007/s11469-020-00305-0.
33.
Shrivastava S.R., Shrivastava P.S. COVID-19 and impairment of mental health: public health perspective. Afr. Health Sci. 2021; 21(4): 1527–1532, doi: 10.4314/ahs.v21i4.5.
34.
Salehi L., Rahimzadeh M., Molaei E., Zaheri H., Esmaelzadeh-Saeieh S. The relationship among fear and anxiety of COVID‐19, pregnancy experience, and mental health disorder in pregnant women: A structural equation model. Brain Behav. 2020; 10(11): e01835, doi: 10.1002/brb3.1835.
35.
El Taha L., Beyrouthy C., Tamim H., Ghazeeri G. Knowledge and attitudes among Lebanese pregnant women and women seeking fertility treatment during the COVID-19 outbreak: a cross-sectional survey. BMJ Open 2022; 12(3): e057873, doi: 10.1136/bmjopen-2021-057873.
36.
Theuring S., Kengonzi A., Hafermann L., Herrmann C., Kabwama S.N., Rubaihayo J. Repercussions of the COVID-19 response in pregnant women in Western Uganda: knowledge, behavior, and emotional state after the first lockdown in 2020. Int. J. Environ. Res. Public Health 2021; 18(15): 7817, doi: 10.3390/ijerph18157817.
37.
Carleton R.N. Fear of the unknown: One fear to rule them all? J. Anxiety Disord. 2016; 41: 5–21, doi: 10.1016/j.janxdis.2016.03.011.
38.
Mizrak Sahin B., Kabakci E.N. The experiences of pregnant women during the COVID-19 pandemic in Turkey: A qualitative study. Women Birth 2021; 34(2): 162–169, doi: 10.1016/j.wombi.2020.09.022.
39.
Ilska M., Kołodziej-Zaleska A., Brandt-Salmeri A., Preis H., Lobel M. Pandemic stress and its correlates among pregnant women during the second wave of COVID-19 in Poland. Int. J. Environ. Res. Public Health 2021; 18(21): 11140, doi: 10.3390/ijerph182111140.
40.
Tomsis Y., Perez E., Sharabi L., Shaked M., Haze S., Hadid S. Postpartum post-traumatic stress symptoms following cesarean section—the mediating effect of sense of control. Psychiatr. Q. 2021; 92(4): 1839–1853, doi: 10.1007/s11126-021-09949-0.
41.
Chen H.H., Lai J.C., Hwang S.J., Huang N., Chou Y.J., Chien L.Y. Understanding the relationship between cesarean birth and stress, anxiety, and depression after childbirth: A nationwide cohort study. Birth 2017; 44(4): 369–376, doi: 10.1111/birt.12295.
42.
Saccone G., Florio A., Aiello F., Venturella R., De Angelis M.C., Locci M. et al. Psychological impact of coronavirus disease 2019 in pregnant women. Am. J. Obstet. Gynecol. 2020; 223(2): 293–295, doi: 10.1016/j.ajog.2020.05.003.
43.
Di Toro F., Gjoka M., Di Lorenzo G., De Santo D., De Seta F., Maso G. et al. Impact of COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin. Microbiol. Infect. 2021; 27(1): 36–46, doi: 10.1016/j.cmi.2020.10.007.
44.
Pichler-Stachl E., Pichler G., Baik N., Urlesberger B., Alexander A., Urlesberger P. et al. Maternal stress after preterm birth: Impact of length of antepartum hospital stay. Women Birth 2016; 29(6): e105–e109, doi: 10.1016/j.wombi.2016.04.008.
45.
Chhari N., Mehta S.C. Stress among patients during hospitalization: A study from Central India. Natl. J. Community Med. 2016; 7(4): 274–277.
46.
Akgor U., Fadıloglu E., Soyak B., Unal C., Cagan M., Temiz B.E. et al. Anxiety, depression and concerns of pregnant women during the COVID-19 pandemic. Arch. Gynecol. Obstet. 2021; 304(1): 125–130, doi: 10.1007/s00404-020-05944-1.
47.
Liu J.M., Chiu F.H., Liu Y.P., Chen S.P., Chan H.H., Yang J.J. et al. Antepartum urinary tract infection and postpartum depression in Taiwan – a nationwide population-based study. BMC Pregnancy Childbirth 2018; 18(1): 79, doi: 10.1186/s12884-018-1692-6.
48.
Farkash E., Weintraub A.Y., Sergienko R., Wiznitzer A., Zlotnik A., Sheiner E. Acute antepartum pyelonephritis in pregnancy: a critical analysis of risk factors and outcomes. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012; 162(1): 24–27, doi: 10.1016/j.ejogrb.2012.01.024.
49.
Verhoeven C.J.M., Boer J., Kok M., Nieuwenhuijze M., de Jonge A., Peters L.L. More home births during the COVID‐19 pandemic in the Netherlands. Birth 2022; 49(4): 792–804, doi: 10.1111/birt.12646.
50.
Cheng R.J., Fisher A.C., Nicholson S.C. Interest in home birth during the COVID‐19 pandemic: Analysis of Google Trends data. J. Midwifery Womens Health 2022; 67(4): 427–434, doi: 10.1111/jmwh.13341.
51.
de Jonge A., Baron R., Westerneng M., Twisk J., Hutton E.K. Perinatal mortality rate in the Netherlands compared to other European countries: a secondary analysis of Euro-PERISTAT data. Midwifery 2013; 29(8): 1011–1018, doi: 10.1016/j.midw.2013.02.005.
52.
Gdańska P., Drozdowicz-Jastrzębska E., Grzechocińska B., Radziwon-Zaleska M., Węgrzyn P., Wielgoś M. Anxiety and depression in women undergoing infertility treatment. Ginekol. Pol. 2017; 88(2): 109–112, doi: 10.5603/GP.a2017.0019.
53.
Kang Y.T., Yao Y., Dou J., Guo X., Li S.Y., Zhao C.N. et al. Prevalence and risk factors of maternal anxiety in late pregnancy in China. Int. J. Environ. Res. Public Health 2016; 13(5): 468, doi: 10.3390/ijerph13050468.
54.
Marquesim N.A., Cavassini A.C., Morceli G., Magalhães C.G., Rudge M.V., Calderon Ide M. et al. Depression and anxiety in pregnant women with diabetes or mild hyperglycemia. Arch. Gynecol. Obstet. 2016; 293(4): 833–837, doi: 10.1007/s00404-015-3838-3.
55.
Jin X., Cheng Z., Yu X., Tao Q., Huang R., Wang S. Continuous supplementation of folic acid in pregnancy and the risk of perinatal depression – A meta-analysis. J. Affect. Disord. 2022; 302: 258–272, doi: 10.1016/j.jad.2022.01.080.
Udostępnij
ARTYKUŁ POWIĄZANY
Śląski Uniwersytet Medyczny w Katowicach, jako Operator Serwisu annales.sum.edu.pl, przetwarza dane osobowe zbierane podczas odwiedzania Serwisu. Realizacja funkcji pozyskiwania informacji o Użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje, zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka), a także poprzez gromadzenie logów serwera www, będącego w posiadaniu Operatora Serwisu. Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług zgodnie z Polityką prywatności.
Możesz wyrazić zgodę na przetwarzanie danych w tych celach, odmówić zgody lub uzyskać dostęp do bardziej szczegółowych informacji.
Możesz wyrazić zgodę na przetwarzanie danych w tych celach, odmówić zgody lub uzyskać dostęp do bardziej szczegółowych informacji.