Bieżący numer
O czasopiśmie
Rada Naukowa
Kolegium Redakcyjne
Polityka prawno-archiwizacyjna
Kodeks etyki publikacyjnej
Wydawca
Informacja o przetwarzaniu danych osobowych w ramach plików cookies oraz subskrypcji newslettera
Archiwum
Dla autorów
Dla recenzentów
Kontakt
Recenzenci
Recenzenci rocznika 2025
Recenzenci rocznika 2024
Recenzenci rocznika 2023
Recenzenci rocznika 2022
Recenzenci rocznika 2021
Recenzenci rocznika 2020
Recenzenci rocznika 2019
Recenzenci rocznika 2018
Recenzenci rocznika 2017
Recenzenci rocznika 2016
Recenzenci rocznika 2015
Recenzenci rocznika 2014
Recenzenci rocznika 2013
Recenzenci rocznika 2012
Polecamy
Śląski Uniwersytet Medyczny w Katowicach
Sklep Wydawnictw SUM
Biblioteka Główna SUM
Polityka prywatności
Deklaracja dostępności
Recenzenci
Recenzenci rocznika 2025
Recenzenci rocznika 2024
Recenzenci rocznika 2023
Recenzenci rocznika 2022
Recenzenci rocznika 2021
Recenzenci rocznika 2020
Recenzenci rocznika 2019
Recenzenci rocznika 2018
Recenzenci rocznika 2017
Recenzenci rocznika 2016
Recenzenci rocznika 2015
Recenzenci rocznika 2014
Recenzenci rocznika 2013
Recenzenci rocznika 2012
Niewydolność serca z zachowaną frakcją wyrzutową lewej komory – perspektywy kliniczne
1
1st Department of Cardiology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
2
Member of the European Reference Network on Heart diseases – ERN GUARD-HEART
Autor do korespondencji
Małgorzata Niemiec
Klinika Kardiologii I Katedry Kardiologii, Śląski Uniwersytet Medyczny w Katowicach, ul. Ziołowa 47, 40-635 Katowice
Klinika Kardiologii I Katedry Kardiologii, Śląski Uniwersytet Medyczny w Katowicach, ul. Ziołowa 47, 40-635 Katowice
Ann. Acad. Med. Siles. 2025;79:181-192
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Niewydolność serca z zachowaną frakcją wyrzutową (heart failure with preserved ejection fraction – HFpEF) jest coraz częściej rozpoznawanym podtypem niewydolności serca, dotykającym głównie osoby starsze i kobiety. Odpowiada za około 51–63% przypadków niewydolności serca, a jej częstość występowania nadal rośnie, głównie ze względu na starzenie się populacji oraz wzrastające obciążenie chorobami współistniejącymi, takimi jak nadciśnienie tętnicze, cukrzyca, otyłość i przewlekła choroba nerek. Wytyczne Europejskiego Towarzystwa Kardiologicznego (European Society of Cardiology – ESC) oraz Amerykańskiego Towarzystwa Kardiologicznego (American Heart Association – AHA) wskazują konieczność spełnienia kryteriów diagnostycznych obejmujących objawy kliniczne, zachowaną frakcję wyrzutową lewej komory (left ventricular ejection fraction – LVEF ≥ 50%), podwyższony poziom peptydów natriuretycznych oraz echokardiograficzne markery dysfunkcji rozkurczowej. Ponadto algorytmy diagnostyczne, takie jak skale HFA-PEFF i H2FPEF, wspomagają różnicowanie HFpEF z innymi chorobami sercowo-naczyniowymi i pozasercowymi. Do niedawna leczenie HFpEF koncentrowało się głównie na łagodzeniu objawów oraz kontrolowaniu chorób współistniejących. Jednak nowsze terapie farmakologiczne wykazały korzyści w zakresie redukcji liczby hospitalizacji oraz poprawy wyników sercowo-naczyniowych. Rokowanie w HFpEF pozostaje niekorzystne; 5-letnia śmiertelność wynosi około 75%. Dlatego pacjenci z HFpEF wymagają kompleksowego postępowania obejmującego modyfikację stylu życia, optymalizację leczenia farmakologicznego oraz ścisłą kontrolę chorób współistniejących. Niniejszy przegląd podsumowuje praktyczne aspekty diagnostyki, patofizjologii, leczenia i rokowania HFpEF, koncentrując się na podejściu interdyscyplinarnym i strategiach wczesnej interwencji, które mogą poprawić wyniki leczenia pacjentów dotkniętych tym wymagającym schorzeniem.
REFERENCJE (66)
1.
Komorowska A., Lelonek M. Heart failure with preserved ejection fraction – the challenge for modern cardiology. Folia Cardiol. 2020; 15(6): 407–412, doi: 10.5603/FC.2020.0060.
2.
Simmonds S.J., Cuijpers I., Heymans S., Jones E.A.V. Cellular and molecular differences between HFpEF and HFrEF: a step ahead in an improved pathological understanding. Cells 2020. 9(1): 242, doi: 10.3390/cells9010242.
3.
Dunlay S.M., Roger V.L., Redfield M.M. Epidemiology of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 2017; 14(10): 591–602, doi: 10.1038/nrcardio.2017.65.
4.
Devereux R.B., Roman M.J., Liu J.E., Welty T.K., Lee E.T., Rodeheffer R. et al. Congestive heart failure despite normal left ventricular systolic function in a population-based sample: the Strong Heart Study. Am. J. Cardiol. 2000; 86(10): 1090–1096, doi: 10.1016/s0002-9149(00)01165-6.
5.
Vasan R.S., Larson M.G., Benjamin E.J., Evans J.C., Reiss C.K., Levy D. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J. Am. Coll. Cardiol. 1999; 33(7): 1948–1955, doi: 10.1016/s0735-1097(99)00118-7.
6.
Kitzman D.W., Gardin J.M., Gottdiener J.S., Arnold A., Boineau R., Aurigemma G. et al. Importance of heart failure with preserved systolic function in patients > or = 65 years of age. CHS Research Group. Cardiovascular Health Study. Am. J. Cardiol. 2001; 87(4): 413–419, doi: 10.1016/s0002-9149(00)01393-x.
7.
Gottdiener J.S., McClelland R.L., Marshall R., Shemanski L., Furberg C.D., Kitzman D.W. et al. Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The Cardiovascular Health Study. Ann. Intern. Med. 2002; 137(8): 631–639, doi: 10.7326/0003-4819-137-8-200210150-00006.
8.
Pfeffer M.A., Shah A.M., Borlaug B.A. Heart failure with preserved ejection fraction in perspective. Circ. Res. 2019; 124(11): 1598–1617, doi: 10.1161/CIRCRESAHA.119.313572.
9.
Pieske B., Tschöpe C., de Boer R.A., Fraser A.G., Anker S.D., Donal E. et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. J. Heart Fail. 2020; 22(3): 391–412, doi: 10.1002/ejhf.1741.
10.
Gerber Y., Weston S.A., Redfield M.M., Chamberlain A.M., Manemann S.M., Jiang R. et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern. Med. 2015; 175(6): 996–1004, doi: 10.1001/jamainternmed.2015.0924.
11.
Chang P.P., Wruck L.M., Shahar E., Rossi J.S., Loehr L.R., Russell S.D. et al. Trends in hospitalizations and survival of acute decompensated heart failure in four US communities (2005–2014): ARIC Study Community Surveillance. Circulation 2018; 138(1): 12–24, doi: 10.1161/CIRCULATIONAHA.117.027551.
12.
Gupta D.K., Shah A.M., Castagno D., Takeuchi M., Loehr L.R., Fox E.R. et al. Heart failure with preserved ejection fraction in African Americans: The ARIC (Atherosclerosis Risk In Communities) study. JACC Heart Fail. 2013; 1(2): 156–163, doi: 10.1016/j.jchf.2013.01.003.
13.
Ather S., Chan W., Bozkurt B., Aguilar D., Ramasubbu K., Zachariah A.A. et al. Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J. Am. Coll. Cardiol. 2012; 59(11): 998–1005, doi: 10.1016/j.jacc.2011.11.040.
14.
Savji N., Meijers W.C., Bartz T.M., Bhambhani V., Cushman M., Nayor M. et al. The association of obesity and cardiometabolic traits with incident HFpEF and HFrEF. JACC Heart Fail. 2018; 6(8): 701–709, doi: 10.1016/j.jchf.2018.05.018.
15.
Lam C.S., Donal E., Kraigher-Krainer E., Vasan R.S. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2011; 13(1): 18–28, doi: 10.1093/eurjhf/hfq121.
16.
Hwang S.J., Melenovsky V., Borlaug B.A. Implications of coronary artery disease in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 2014; 63(25 Pt A): 2817–2827, doi: 10.1016/j.jacc.2014.03.034.
17.
Kupari M., Lindroos M., Iivanainen A.M., Heikkilä J., Tilvis R. Congestive heart failure in old age: prevalence, mechanisms and 4-year prognosis in the Helsinki Ageing Study. J. Intern. Med. 1997; 241(5): 387–394, doi: 10.1046/j.1365-2796.1997.129150000.x.
18.
Lam C.S.P., Voors A.A., de Boer R.A., Solomon S.D., van Veldhuisen D.J. Heart failure with preserved ejection fraction: from mechanisms to therapies. Eur. Heart J. 2018; 39(30): 2780–2792, doi: 10.1093/eurheartj/ehy301.
19.
King M., Kingery J., Casey B. Diagnosis and evaluation of heart failure. Am. Fam. Physician 2012; 85(12): 1161–1168.
20.
Madhok V., Falk G., Rogers A., Struthers A.D., Sullivan F.M., Fahey T. The accuracy of symptoms, signs and diagnostic tests in the diagnosis of left ventricular dysfunction in primary care: a diagnostic accuracy systematic review. BMC Fam. Pract. 2008; 9: 56, doi: 10.1186/1471-2296-9-56.
21.
Anjan V.Y., Loftus T.M., Burke M.A., Akhter N., Fonarow G.C., Gheorghiade M. et al. Prevalence, clinical phenotype, and outcomes associated with normal B-type natriuretic peptide levels in heart failure with preserved ejection fraction. Am. J. Cardiol. 2012; 110(6): 870–876, doi: 10.1016/j.amjcard.2012.05.014.
22.
Mulrow C.D., Lucey C.R., Farnett L.E. Discriminating causes of dyspnea through clinical examination. J. Gen. Intern. Med. 1993; 8(7): 383–392, doi: 10.1007/BF02600079.
23.
Wang C.S., FitzGerald J.M., Schulzer M., Mak E., Ayas N.T. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA 2005; 294(15): 1944–1956, doi: 10.1001/jama.294.15.1944.
24.
Shah S.J., Kitzman D.W., Borlaug B.A., van Heerebeek L., Zile M.R., Kass D.A. et al. Phenotype‐specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation 2016; 134(1): 73–90, doi: 10.1161/CIRCULATIONAHA.116.021884.
25.
Upadhya B., Kitzman D.W. Heart failure with preserved ejection fraction: New approaches to diagnosis and management. Clin. Cardiol. 2020; 43(2): 145–155, doi: 10.1002/clc.23321.
26.
Heidenreich P.A., Bozkurt B., Aguilar D., Allen L.A., Byun J.J., Colvin M.M. et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022; 145(18): e876–e894, doi: 10.1161/CIR.0000000000001062.
27.
McDonagh T.A., Metra M., Adamo M., Gardner R.S., Baumbach A., Böhm M. et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2023; 44(37): 3627–3639, doi: 10.1093/eurheartj/ehad195.
28.
Pagel P.S., Tawil J.N., Boettcher B.T., Izquierdo D.A., Lazicki T.J., Crystal G.J. et al. Heart failure with preserved ejection fraction: A comprehensive review and update of diagnosis, pathophysiology, treatment, and perioperative implications. J. Cardiothorac. Vasc. Anesth. 2021; 35(6): 1839–1859, doi: 10.1053/j.jvca.2020.07.016.
29.
Redfield M.M. Heart failure with preserved ejection fraction. N. Engl. J. Med. 2016; 375(19): 1868–1877, doi: 10.1056/NEJMcp1511175.
30.
Hagendorff A., Stöbe S., Kandels J., de Boer R., Tschöpe C. Diagnostic role of echocardiography for patients with heart failure symptoms and preserved left ventricular ejection fraction. Herz 2022; 47(4): 293–300, doi: 10.1007/s00059-022-05118-6.
31.
Paulus W.J., Tschöpe C., Sanderson J.E., Rusconi C., Flachskampf F.A., Rademakers F.E. et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur. Heart J. 2007; 28(20): 2539–2550, doi: 10.1093/eurheartj/ehm037.
32.
Berni A., Cappelli F., Bitossi L., Cecioni I., Cappelli B., Toncelli L. et al. Non-invasive tissue Doppler imaging pulmonary capillary wedge pressure measurement improves NT-proBNP prognostic value in heart failure. Acta Cardiol. 2009; 64(2): 213–218, doi: 10.2143/AC.64.2.2036140.
33.
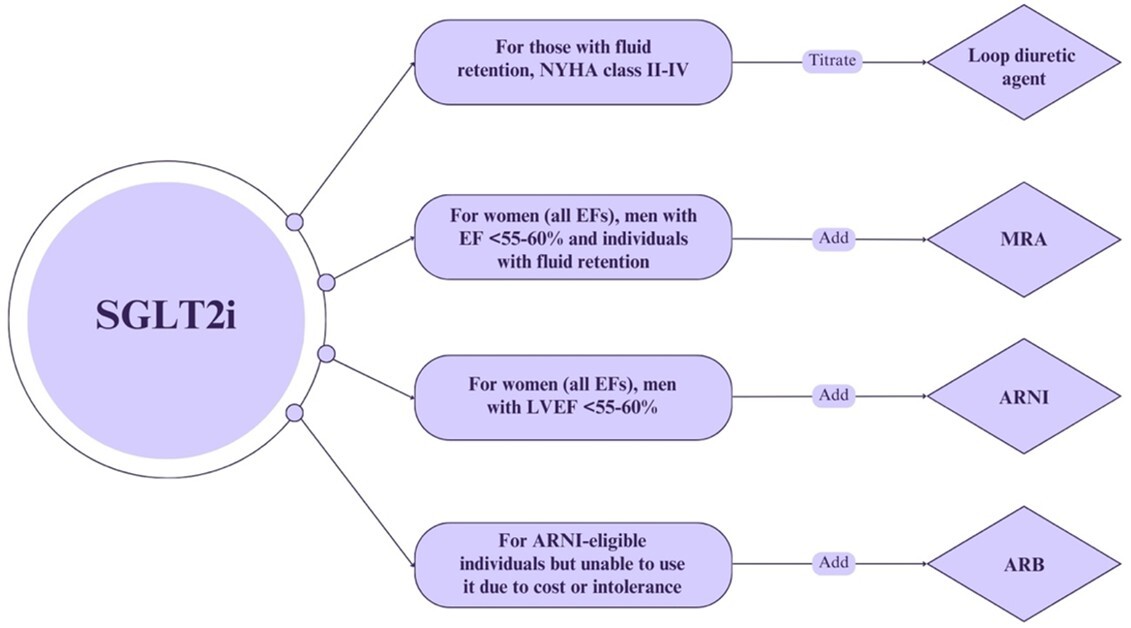
Kittleson M.M., Panjrath G.S., Amancherla K., Davis L.L., Deswal A., Dixon D.L. et al. 2023 ACC Expert Consensus Decision Pathway on management of heart failure with preserved ejection fraction: A report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 2023; 81(18): 1835–1878, doi: 10.1016/j.jacc.2023.03.393.
34.
Kasahara S., Sakata Y., Nochioka K., Yamauchi T., Onose T., Tsuji K. et al. Comparable prognostic impact of BNP levels among HFpEF, Borderline HFpEF and HFrEF: a report from the CHART-2 Study. Heart Vessels 2018; 33(9): 997–1007, doi: 10.1007/s00380-018-1150-4.
35.
Wang T.J., Larson M.G., Levy D., Benjamin E.J., Leip E.P., Wilson P.W. et al. Impact of obesity on plasma natriuretic peptide levels. Circulation 2004; 109(5): 594–600, doi: 10.1161/01.CIR.0000112582.16683.EA.
36.
Obokata M., Reddy Y.N.V., Pislaru S.V., Melenovsky V., Borlaug B.A. Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation 2017; 136(1): 6–19, doi: 10.1161/CIRCULATIONAHA.116.026807.
37.
Oikonomou E., Zografos T., Papamikroulis G.A., Siasos G., Vogiatzi G., Theofilis P. et al. Biomarkers in atrial fibrillation and heart failure. Curr. Med. Chem. 2019; 26(5): 873–887, doi: 10.2174/0929867324666170830100424.
38.
Guazzi M., Wilhelm M., Halle M., Van Craenenbroeck E., Kemps H., de Boer R.A. et al. Exercise testing in heart failure with preserved ejection fraction: an appraisal through diagnosis, pathophysiology and therapy – A clinical consensus statement of the Heart Failure Association and European Association of Preventive Cardiology of the European Society of Cardiology. Eur. J. Heart Fail. 2022; 24(8): 1327–1345, doi: 10.1002/ejhf.2601.
39.
Dorfs S., Zeh W., Hochholzer W., Jander N., Kienzle R.P., Pieske B. et al. Pulmonary capillary wedge pressure during exercise and long-term mortality in patients with suspected heart failure with preserved ejection fraction. Eur. Heart J. 2014; 35(44): 3103–3112, doi: 10.1093/eurheartj/ehu315.
40.
Huang W., Resch S., Oliveira R.K., Cockrill B.A., Systrom D.M., Waxman A.B. Invasive cardiopulmonary exercise testing in the evaluation of unexplained dyspnea: Insights from a multidisciplinary dyspnea center. Eur. J. Prev. Cardiol. 2017; 24(11): 1190–1199, doi: 10.1177/2047487317709605.
41.
Reddy Y.N.V., Carter R.E., Obokata M., Redfield M.M., Borlaug B.A. A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation 2018; 138(9): 861–870, doi: 10.1161/CIRCULATIONAHA.118.034646.
42.
Ponikowski P., Voors A.A., Anker S.D., Bueno H., Cleland J.G.F., Coats A.J.S. et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. [Article in Polish]. Kardiol. Pol. 2016; 74(10): 1037–1147, doi: 10.5603/KP.2016.0141.
43.
McMurray J.J., Adamopoulos S., Anker S.D., Auricchio A., Böhm M., Dickstein K. et. al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2012; 33(14): 1787–1847, doi: 10.1093/eurheartj/ehs104.
44.
Maisel A., Mueller C., Adams K. Jr, Anker S.D., Aspromonte N., Cleland J.G. et. al. State of the art: using natriuretic peptide levels in clinical practice. Eur. J. Heart Fail. 2008; 10(9): 824–839, doi: 10.1016/j.ejheart.2008.07.014.
45.
Jin X., Nauta J.F., Hung C.L., Ouwerkerk W., Teng T.K., Voors A.A. et al. Left atrial structure and function in heart failure with reduced (HFrEF) versus preserved ejection fraction (HFpEF): systematic review and meta-analysis. Heart Fail. Rev. 2022; 27(5): 1933–1955, doi: 10.1007/s10741-021-10204-8.
46.
Gupta A., Whiteley W.N., Godec T., Rostamian S., Ariti C., Mackay J. et al. Legacy benefits of blood pressure treatment on cardiovascular events are primarily mediated by improved blood pressure variability: the ASCOT trial. Eur. Heart J. 2024; 45(13): 1159–1169, doi: 10.1093/eurheartj/ehad814.
47.
Gupta A., Mackay J., Whitehouse A., Godec T., Collier T., Pocock S. et al. Long-term mortality after blood pressure-lowering and lipid-lowering treatment in patients with hypertension in the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) Legacy study: 16-year follow-up results of a randomised factorial trial. Lancet 2018; 392(10153): 1127–1137, doi: 10.1016/S0140-6736(18)31776-8.
48.
Glezer M.G.; FORSAGE Investigators. Antihypertensive effectiveness of perindopril arginine and indapamide single-pill combination according to body mass index: findings from the FORSAGE study. Cardiol. Ther. 2020; 9(1): 139–152, doi: 10.1007/s40119-020-00162-x.
49.
Mazza A., Townsend D.M., Schiavon L., Torin G., Lenti S., Rossetti C. et al. Long-term effect of the perindopril/indapamide/amlodipine single-pill combination on left ventricular hypertrophy in outpatient hypertensive subjects. Biomed. Pharmacother. 2019; 120: 109539, doi: 10.1016/j.biopha.2019.109539.
50.
Cicero A.F.G., Fogacci F., Rizzoli E., D’Addato S., Borghi C. Long-term impact of different triple combination antihypertensive medications on blood pressure control, metabolic pattern and incident events: data from the Brisighella Heart Study. J. Clin. Med. 2021; 10(24): 5921, doi: 10.3390/jcm10245921.
51.
Snyman J.R., Bortolotto L.A., Degli Esposti L., Jayagopal P.B., Konradi A.O., Perrone V. et al. A real-world analysis of outcomes and healthcare costs of patients on perindopril/indapamide/amlodipine single-pill vs. multiple-pill combination in Italy. J. Hypertens. 2024; 42(1): 136–142, doi: 10.1097/HJH.0000000000003570.
52.
Masi S., Kobalava Z., Veronesi C., Giacomini E., Degli Esposti L., Tsioufis K. A retrospective observational real-world analysis of the adherence, healthcare resource consumption and costs in patients treated with bisoprolol/perindopril as single-pill or free combination. Adv. Ther. 2024; 41(1): 182–197, doi: 10.1007/s12325-023-02707-7.
53.
Tridetti J., Nguyen Trung M.L., Ancion A., Lancellotti P. The PARAGON-HF trial. [Article in French]. Rev. Med. Liege 2020; 75(2): 130–135.
54.
Anker S.D., Siddiqi T.J., Filippatos G., Zannad F., Ferreira J.P., Pocock S.J. et al. Outcomes with empagliflozin in heart failure with preserved ejection fraction using DELIVER-like endpoint definitions. Eur. J. Heart Fail. 2022; 24(8): 1400–1405, doi: 10.1002/ejhf.2558.
55.
Prausmüller S., Weidenhammer A., Heitzinger G., Spinka G., Goliasch G., Arfsten H. et al. Obesity in heart failure with preserved ejection fraction with and without diabetes: risk factor or innocent bystander? Eur. J. Prev. Cardiol. 2023; 30(12): 1247–1254, doi: 10.1093/eurjpc/zwad140.
56.
Banerjee D., Wang A.Y. Personalizing heart failure management in chronic kidney disease patients. Nephrol. Dial. Transplant. 2022; 37(11): 2055–2062, doi: 10.1093/ndt/gfab026.
57.
Lang C.C., Smith K., Wingham J., Eyre V., Greaves C.J., Warren F.C. et al. A randomised controlled trial of a facilitated home-based rehabilitation intervention in patients with heart failure with preserved ejection fraction and their caregivers: the REACH-HFpEF Pilot Study. BMJ Open 2018; 8(4): e019649, doi: 10.1136/bmjopen-2017-019649.
58.
Zakeri R., Chamberlain A.M., Roger V.L., Redfield M.M. Temporal relationship and prognostic significance of atrial fibrillation in heart failure patients with preserved ejection fraction: a community-based study. Circulation 2013; 128(10): 1085–1093, doi: 10.1161/CIRCULATIONAHA.113.001475.
59.
Mehra M.R., Vaduganathan M., Fu M., Ferreira J.P., Anker S.D., Cleland J.G.F. et al. A comprehensive analysis of the effects of rivaroxaban on stroke or transient ischaemic attack in patients with heart failure, coronary artery disease, and sinus rhythm: the COMMANDER HF trial. Eur. Heart J. 2019; 40(44): 3593–3602, doi: 10.1093/eurheartj/ehz427.
60.
Crespo-Leiro M.G., Anker S.D., Maggioni A.P., Coats A.J., Filippatos G., Ruschitzka F. et al. European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur. J. Heart Fail. 2016; 18(6): 613–625, doi: 10.1002/ejhf.566.
61.
Rich J.D., Burns J., Freed B.H., Maurer M.S., Burkhoff D., Shah S.J. Meta-Analysis Global Group in Chronic (MAGGIC) Heart Failure Risk Score: Validation of a simple tool for the prediction of morbidity and mortality in heart failure with preserved ejection fraction. J. Am. Heart Assoc. 2018; 7(20): e009594, doi: 10.1161/JAHA.118.009594.
62.
Solomon S.D., McMurray J.J.V., Anand I.S., Ge J., Lam C.S.P., Maggioni A.P. et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N. Engl. J. Med. 2019; 381(17): 1609–1620, doi: 10.1056/NEJMoa1908655.
63.
Solomon S.D., Zile M., Pieske B., Voors A., Shah A., Kraigher-Krainer E. et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet 2012; 380(9851): 1387–1395, doi: 10.1016/S0140-6736(12)61227-6.
64.
Fudim M., Kelly J.P., Brophy T.J., DeVore A.D., Hammill B.G., Peterson E.D. et al. Trends in treatment for patients hospitalized with heart failure with preserved ejection fraction before and after treatment of preserved cardiac function heart failure with an aldosterone antagonist (TOPCAT). Am. J. Cardiol. 2020; 125(11): 1655–1660, doi: 10.1016/j.amjcard.2020.02.038.
65.
Yusuf S., Pfeffer M.A., Swedberg K., Granger C.B., Held P., McMurray J.J. et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet 2003; 362(9386): 777–781, doi: 10.1016/S0140-6736(03)14285-7.
66.
Spertus J.A., Jones P.G., Sandhu A.T., Arnold S.V. Interpreting the Kansas City Cardiomyopathy Questionnaire in clinical trials and clinical care: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020; 76(20): 2379–2390, doi: 10.1016/j.jacc.2020.09.542.
Udostępnij
ARTYKUŁ POWIĄZANY
Śląski Uniwersytet Medyczny w Katowicach, jako Operator Serwisu annales.sum.edu.pl, przetwarza dane osobowe zbierane podczas odwiedzania Serwisu. Realizacja funkcji pozyskiwania informacji o Użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje, zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka), a także poprzez gromadzenie logów serwera www, będącego w posiadaniu Operatora Serwisu. Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług zgodnie z Polityką prywatności.
Możesz wyrazić zgodę na przetwarzanie danych w tych celach, odmówić zgody lub uzyskać dostęp do bardziej szczegółowych informacji.
Możesz wyrazić zgodę na przetwarzanie danych w tych celach, odmówić zgody lub uzyskać dostęp do bardziej szczegółowych informacji.